Ischemia Reperfusion Injury in Orthotopic Liver Transplantation Primes the Adaptive Immune Response and Generation of Proinflammatory Cytokines
1Surgery, University of California, Los Angeles, Los Angeles, CA
2Pathology and Lab Medicine, University of California, Los Angeles, Los Angeles, CA.
Meeting: 2015 American Transplant Congress
Abstract number: C282
Keywords: Graft function, Inflammation, Ischemia, Liver transplantation
Session Information
Session Name: Poster Session C: Translational Biomarkers and Immune Monitoring
Session Type: Poster Session
Date: Monday, May 4, 2015
Session Time: 5:30pm-6:30pm
 Presentation Time: 5:30pm-6:30pm
Presentation Time: 5:30pm-6:30pm
Location: Exhibit Hall E
Background: Transplanted organs are exquisitely susceptible to effects of ischemia/reperfusion injury (IRI), an immune-mediated process that occurs during transplantation and beyond. Recipient and graft outcomes, including early dysfunction and late rejection, are greatly affected by IRI.
Methods: To understand the relevance of immunologic and inflammatory factors in the peri- and post-transplant period to recipient and graft outcomes, we collected blood and tissues from 27 adult cadaveric liver transplant recipients. We collected blood from the central venous system and from the operative field during the transplant operation. Post-transplant we collected blood on day 1, weekly for 1 month, bi-monthly for 3 months, monthly for 6 months, and quarterly until 24 months. We obtained graft biopsies before and after reperfusion. Plasma samples were analyzed using Luminex 38-plex chemokine and cytokine arrays (Millipore). We also developed a novel scheme to grade reperfusion injury in liver grafts. Biopsy grading of IRI (0=none to 4=severe) was based on the following parameters: necrosis, inflammatory infiltrates, large droplet macrovesicular steatosis, congestion, and ballooning. IRI scores and cytokine levels were subjected to statistical analysis to detect significant associations.
Results: 12 of 27 patients (44%) had mild to severe reperfusion injury (IRI score ≥2 out of 4) on biopsy. These patients had significantly higher levels of IL-17A on post-operative day 7 than patients with no to minimal reperfusion injury (IRI score 0 or 1). They also had higher levels of interferon-γ on post-operative day 7 (Figure 1). 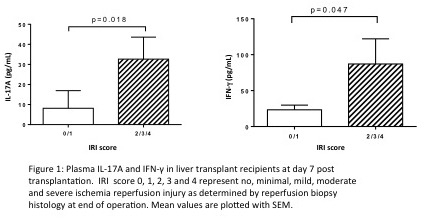
Conclusion: We conclude that increased plasma IL-17A and interferon-γ was correlated with increased IRI. These results imply that innate immune-mediated processes act as a trigger and/or amplifier of the adaptive response leading to generation of proinflammatory cytokines.
To cite this abstract in AMA style:
Zarrinpar A, Rao P, Lassman C, Agopian V, Kaldas F, Farmer D, Busuttil R, Zhai Y, Kupiec-Weglinski J, Reed E. Ischemia Reperfusion Injury in Orthotopic Liver Transplantation Primes the Adaptive Immune Response and Generation of Proinflammatory Cytokines [abstract]. Am J Transplant. 2015; 15 (suppl 3). https://atcmeetingabstracts.com/abstract/ischemia-reperfusion-injury-in-orthotopic-liver-transplantation-primes-the-adaptive-immune-response-and-generation-of-proinflammatory-cytokines/. Accessed July 12, 2025.« Back to 2015 American Transplant Congress
