Activation of Innate Immunity During Human OLT-IRI Triggers Adaptive Immunity and Correlates with the Degree of IRI Injury.
1Surgery, Dumont-UCLA Transplant Ctr, Los Angeles, CA
2Pathology, UCLA, Los Angeles, CA.
Meeting: 2016 American Transplant Congress
Abstract number: C124
Keywords: Immunogenicity, Inflammation, Ischemia, Lung transplantation
Session Information
Session Name: Poster Session C: Ischemia Reperfusion Injury and Organ Preservation
Session Type: Poster Session
Date: Monday, June 13, 2016
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Halls C&D
Ischemia reperfusion injury (IRI) in orthotopic liver transplantation (OLT) can severely compromise graft and recipient survival. We postulate this is mediated by interactions between the innate and adaptive arms of the immune system. To determine the evolution of cytokine responses following OLT, we collected blood from 53 adult OLT recipients serially: pre-operative, intraoperative blood liver flush (LF), and post-transplant on day 1, weekly for 1 month, and bi-monthly for 3 months. Graft biopsies were collected pre-transplant and 2 hours after reperfusion. Samples were analyzed using cytokine/chemokine arrays. Liver biopsies were graded for IRI (0=none to 4=severe) based on necrosis, inflammatory infiltrates, steatosis, congestion, and ballooning. A clinical IRI score based on post-transplant AST and ALT levels within the first week was used to derive an independent ranking system. 47% of transplant recipients (25/53) were IRI+ (score >2 by histopathology). IRI+ patients showed increased expression of the pro-inflammatory cytokines TNFa, IL-2, IL-8, IL-7, EGF pre-operatively. The intraoperative liver flush from IRI+ patients showed increases in innate immune cytokines IL-2, IL-8, IL-12p70 and IL-3. Early post transplant (day1) adaptive cytokines/chemokines IL-13 and IL-17a were significantly higher in IRI+ patients compared to IRI-. Late after IRI (post-week 1 and 4), adaptive cytokines/chemokines dominate the immune response in IRI+ recipients showing significant increases in IL-17a, IL-2, IL-4, IL-7, IL-3 and eotaxin. Persistent IL-1Ra was found in IRI+ recipients across most time-points tested. IRI+ patients exhibited increased IL-1a expression at week 1 post transplant that was accompanied by a significant decrease in IL-1Ra implying a resurgence of an acute inflammatory response. Three cytokines were similarly increased when analyzed by the clinical score (IL-3, IL-5, and IL-1Ra). Knowledge of innate and adaptive immunophenotypes in IRI will improve patient/donor management and refine therapeutic interventions. 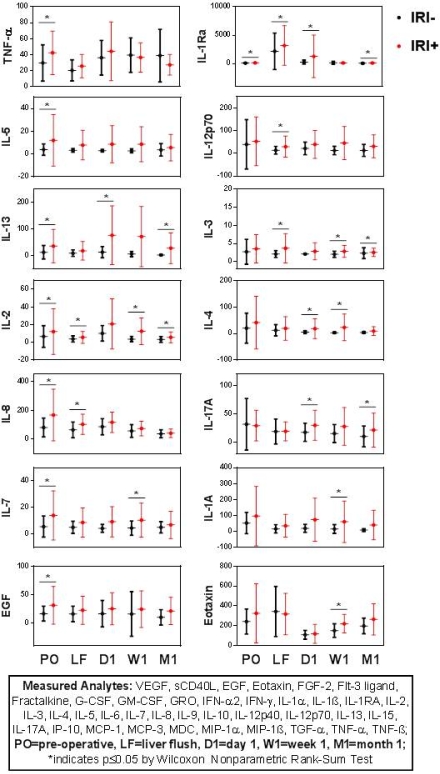
CITATION INFORMATION: Zarrinpar A, Sosa R, Rao P, Lassman C, Busuttil R, Gjertson D, Kupiec-Weglinski J, Reed E. Activation of Innate Immunity During Human OLT-IRI Triggers Adaptive Immunity and Correlates with the Degree of IRI Injury. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Zarrinpar A, Sosa R, Rao P, Lassman C, Busuttil R, Gjertson D, Kupiec-Weglinski J, Reed E. Activation of Innate Immunity During Human OLT-IRI Triggers Adaptive Immunity and Correlates with the Degree of IRI Injury. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/activation-of-innate-immunity-during-human-olt-iri-triggers-adaptive-immunity-and-correlates-with-the-degree-of-iri-injury/. Accessed February 16, 2026.« Back to 2016 American Transplant Congress
