The Impact of Thrombin / Protease-Activated Receptor-1 Pathway in Hepatic Ischemia-Reperfusion Injury in Mice
Hepatobiliary Pancreatic and Transplant Surgery, Mie University Graduate School of Medicine, Tsu City, Mie, Japan
Meeting: 2019 American Transplant Congress
Abstract number: B30
Keywords: Apoptosis, Inflammation, Ischemia, Liver
Session Information
Session Name: Poster Session B: Ischemia Reperfusion & Organ Rehabilition
Session Type: Poster Session
Date: Sunday, June 2, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
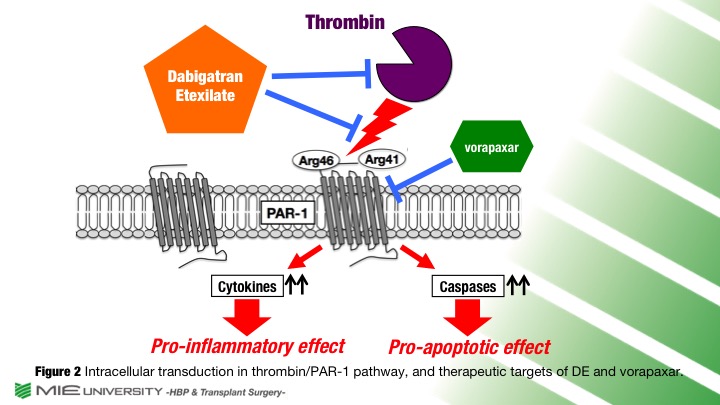
Location: Hall C & D
*Purpose: Coagulation cascade is an important pathway in the pathophysiology of hepatic ischemia-reperfusion injury(IRI). Generation of thrombin is a critical factor of coagulation induced by liver injury. Thrombin not only cleaves fibrinogen, but also triggers inflammatory and apoptotic signaling via an activation of thrombin receptor, protease-activated receptor-1(PAR-1). There are few studies on thrombin/PAR-1 pathway in hepatic IRI. The direct thrombin antagonist, dabigatran etexilate(DE), is a direct oral anti-coagulant(DOAC) and clinically used for several thrombosis. DE binds to the active site of thrombin and downregulates the thrombin/PAR-1 pathway without influence on other coagulant factors. In this study, we aimed to clarify possible protective effects and underlying mechanisms of DE against hepatic IRI, by comparing the effect of PAR-1 antagonist, vorapaxar(VR).
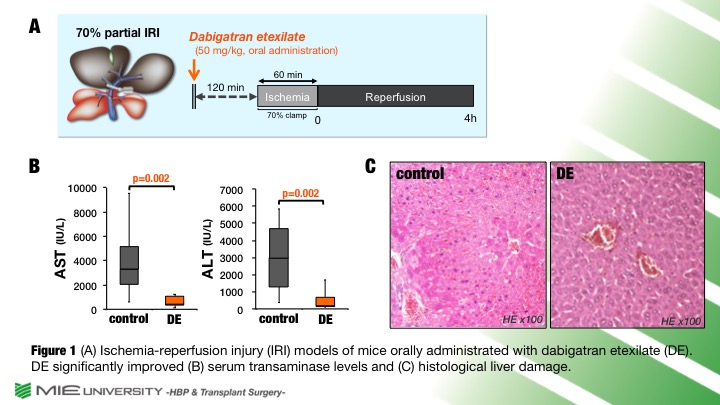
*Methods: Using partial hepatic IRI model of mice, plasma thrombin-antithrombin complex(TAT) levels were evaluated. Subsequently, mice were orally administrated with or without DE(50 mg/kg) before IRI. Additionally, mice were intraperitoneally administrated with or without VR(5μg/kg) before and after IRI.
*Results: Plasma TAT levels, which were equivalent to thrombin levels, were significantly increased after IRI compared to naïve liver (0.01 [0-0.11] in naïve vs. 4.56 [3.05-7.54] ng/ml in IRI, p=0.004). DE significantly improved serum transaminase levels and histological liver damage (AST: 3,304 [2,059-5,146] in control vs. 422 [346-1,073] IU/L in DE, p=0.002; Suzuki’s score: 5.6 [3.6-6.6] in control. vs. 1.8 [1.8-2.4] in DE, p=0.003). VR significantly improved serum transaminase levels and histological liver damage (AST: 3,109 [2,766-3,665] in control vs. 1808 [1,593-2,131] IU/L in VR, p=0.006; Suzuki’s score: 6.5 [5.4-7.1] in control vs. 2.8 [2.0-3.9] in VR, p=0.004).
*Conclusions: Hepatic IRI increased a generation of thrombin. Direct inhibitions of thrombin by DE and PAR-1 by VR significantly attenuated hepatic IRI. We consider that the thrombin/PAR-1 pathway may be a new therapeutic target on hepatic IRI.
To cite this abstract in AMA style:
Noguchi D, Kuriyama N, Fujii T, Kato H, Kishiwada M, Mizuno S, Usui M, Sakurai H, Isaji S. The Impact of Thrombin / Protease-Activated Receptor-1 Pathway in Hepatic Ischemia-Reperfusion Injury in Mice [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/the-impact-of-thrombin-protease-activated-receptor-1-pathway-in-hepatic-ischemia-reperfusion-injury-in-mice/. Accessed February 28, 2026.« Back to 2019 American Transplant Congress