Differing Gene Expression Profiles and Signaling Pathways Observed Between Alloreactive and Tolerant T Cells in a Recipient Following Bilateral Orthotopic Lung Transplant (BOLT) and Bone Marrow Transplant (BMT) from the Same Cadaveric UNOS Donor
UPMC Children's Hospital of Pittsburgh, Pittsburgh, PA
Meeting: 2022 American Transplant Congress
Abstract number: 1278
Keywords: Bone marrow transplantation, Gene expression, Lung transplantation, Tolerance
Topic: Basic Science » Basic Science » 12 - Immunosuppression & Tolerance: Preclinical & Translational Studies
Session Information
Session Name: Immunosuppression & Tolerance: Preclinical & Translational Studies
Session Type: Poster Abstract
Date: Monday, June 6, 2022
Session Time: 7:00pm-8:00pm
 Presentation Time: 7:00pm-8:00pm
Presentation Time: 7:00pm-8:00pm
Location: Hynes Halls C & D
*Purpose: Primary immunodeficiency (PID) patients may develop pulmonary complications, and most are ineligible for either BOLT or BMT due to futility. A prospective trial in PID with end-stage lung disease (NCT01852370) tests our hypothesis that persistent engraftment of cadaveric lung donor vertebral body (VB) marrow stem cells could restore immunity and result in lifelong tolerance.
*Methods: A 14 year old female (IL7R– SCID) underwent BMT 4m after BOLT from a 1/8 HLA-allele matched donor. Marrow suspension from VB was CD3+/CD19+depleted and cryopreserved. We have previously shown reduced proliferative, cytotoxic and cytokine responses 2yrs post-BMT (1yr off ISD). Peripheral regulatory mechanism(s) were examined by depletion of Tregs, blocking the IL10R or adding low dose IL2 to break anergy. T-cell receptor (TCR)β repertoires of alloreactive T-cell clones were assessed for clonal deletion using ImmunoSEQ™. Gene expression profiling and signaling pathway analysis on alloreactive or tolerant T cells were performed using RNA-sequencing and software of CLC Genomic Workbench®v21, GSEA®v4.1.0 and IPA®.
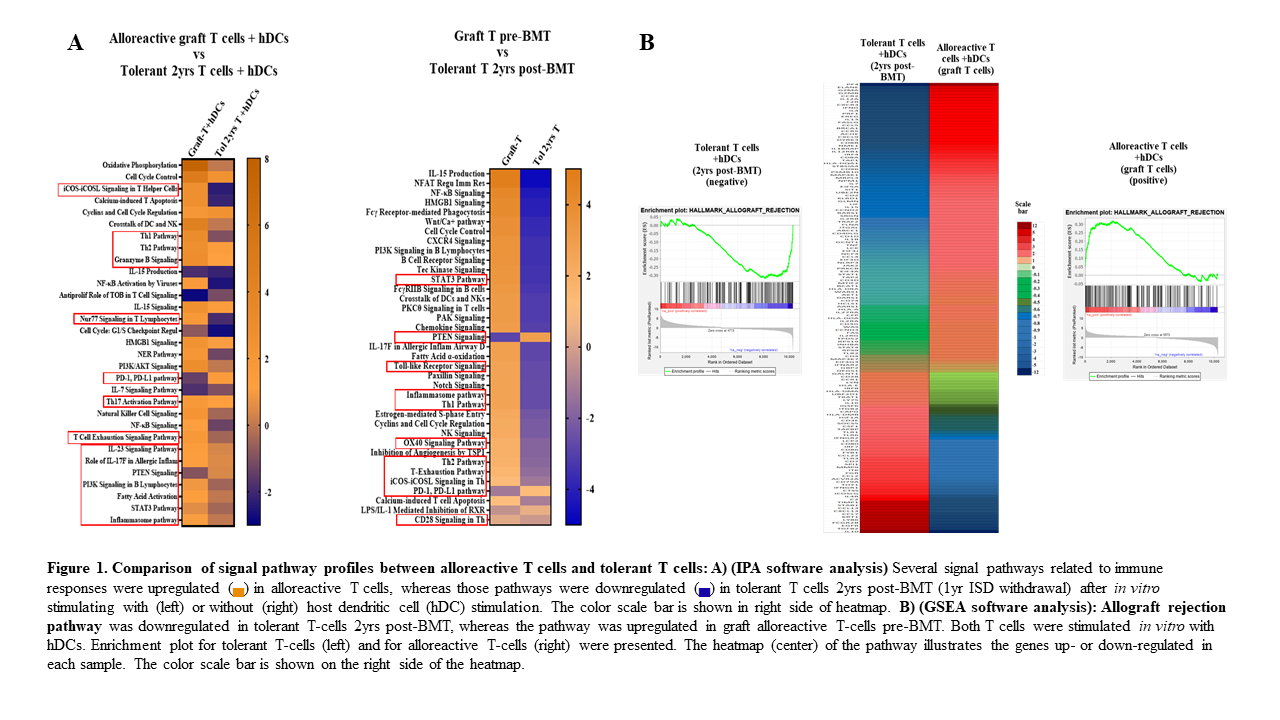
*Results: Initially, she engrafted with 100% donor cells. Declining donor chimerism (CD33+ myeloid 60-70% or CD3+T-cell ~27% donor) prompted donor leukocyte infusion ~10w post-BMT. Myeloid chimerism settled between 7-14% during years 2-5 while T-cells remained >95% donor. T/B cells, TCR/BCR repertoires, and sjTREC exceeded pre-BMT values by 3-6m. She was off ISD by 1yr post-BMT and serial lung biopsies detected no rejection. Circulating donor T-cells 2yrs post-BMT were hyporesponsive to host DCs while vigorously responding to 3rd party APCs. Treg depletion or IL10R blocking did not lead to rebound alloreactivity. TCRβ ImmunoSEQ® revealed the gradual disappearance of host reactive clones that remained undetectable even following exogenous IL2. Unlike T-cells from the marrow graft, tolerant T-cells in circulation presented distinct patterns of gene expressions, with downregulation of allograft rejection and T-helper response, co-stimulation, cell proliferation pathways paired with upregulation of co-inhibition and PTEN pathways (Fig1).
*Conclusions: This is the first case to demonstrate successful engraftment, immune competence, and acquisition of long-term tolerance from deceased organ donor VB marrow. Tolerance was characterized by clonal deletion of alloreactive T cells, along with altered signaling pathways in tolerant T-cells.
To cite this abstract in AMA style:
Szabolcs P, Garchar E, Rajasundaram D, Chen X. Differing Gene Expression Profiles and Signaling Pathways Observed Between Alloreactive and Tolerant T Cells in a Recipient Following Bilateral Orthotopic Lung Transplant (BOLT) and Bone Marrow Transplant (BMT) from the Same Cadaveric UNOS Donor [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/differing-gene-expression-profiles-and-signaling-pathways-observed-between-alloreactive-and-tolerant-t-cells-in-a-recipient-following-bilateral-orthotopic-lung-transplant-bolt-and-bone-marrow-transp/. Accessed February 16, 2026.« Back to 2022 American Transplant Congress