The Impact of Microcirculation Inflammation in Predicting Treatment Response for Late Onset Antibody Mediated Rejection
1Department of Transplantation Surgery, Yonsei University Health System, Seoul, Republic of Korea
2Department of Pathology, Yonsei University Health System, Seoul, Republic of Korea
3Department of Internal Medicine, Yonsei University Health System, Seoul, Republic of Korea
4Department of Surgery, CHA Bundang Medical Center, Bundang, Republic of Korea.
Meeting: 2015 American Transplant Congress
Abstract number: A109
Keywords: Antibodies, Biopsy, Microcirculation, Rejection
Session Information
Session Name: Poster Session A: Kidney Antibody Mediated Rejection
Session Type: Poster Session
Date: Saturday, May 2, 2015
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Exhibit Hall E
Background
There have been marked advances of immunosuppression. However, management of late onset antibody-mediated rejection (AMR) after 6 months is still challenging. Despite important diagnostic and prognostic role of microcirculation inflammation (MI; defined by the addition of glomerulitis score and peritubular capillaritis score) in AMR, there is no data of the impact of MI score in predicting treatment response.
Methods
Late onset AMR was diagnosed using Banff 2007 criteria. We exclude patients with estimated glomerular filtration rates (eGFR; MDRD) less than 15ml/minute/1.73m2 at the time of diagnosis. Patients were categorized by MI score. Responses to therapy were assessed by eGFR at 6 month after treatment compared to eGFR at diagnosis of AMR; complete response if the eGFR improved more than 10%, no response if the eGFR declined over 10%, and partial response if cases fell between the extremes.
Results
A total of 27 patients were treated with AMR between 2011 and 2014. All patients were treated with plasmapheresis. Twenty six recipients (96.3%) received low dose intravenous immunoglobulin and/or rituximab. We divided the patients into three groups according to MI score assessed on the biopsy; MI 0 (n=7), MI 1-2 (n=12), and MI>3 (n=8). Based on our response criteria, 8 patients (3 of MI 0, 3 of MI 1-2, 2 of MI≥3) showed complete response, and 11 patients (4 of MI 0, 5 of MI 1-2, 2 of MI≥3) showed no response (p=0.735).
Conclusion
In late onset AMR after kidney transplantation, MI score could not predict the treatment response.
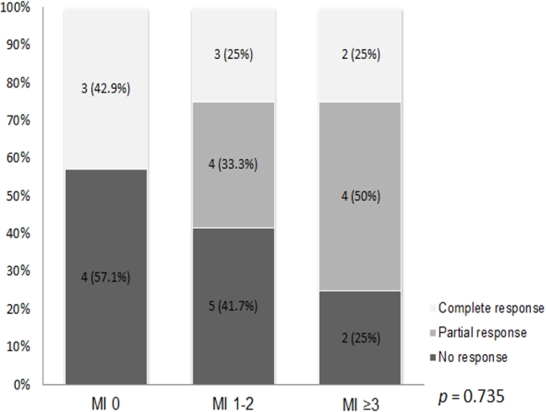 Treatment response of antibody-mediated rejection according to MI score
Treatment response of antibody-mediated rejection according to MI score
To cite this abstract in AMA style:
Lee J, Lee J, Lim B, Kim B, Ju M, Kim M, Kim S, Kim Y, Jeong H, Park K, Huh K. The Impact of Microcirculation Inflammation in Predicting Treatment Response for Late Onset Antibody Mediated Rejection [abstract]. Am J Transplant. 2015; 15 (suppl 3). https://atcmeetingabstracts.com/abstract/the-impact-of-microcirculation-inflammation-in-predicting-treatment-response-for-late-onset-antibody-mediated-rejection/. Accessed July 18, 2025.« Back to 2015 American Transplant Congress
