Molecular Correlates of Atrophy-Fibrosis in Human Kidney Transplants Provides a New Model of Renal Fibrosis
University of Alberta, Edmonton, Canada.
Meeting: 2015 American Transplant Congress
Abstract number: 375
Keywords: B cells, Fibrosis, Inflammation, Renal injury
Session Information
Session Name: Concurrent Session: Kidney: Antibodies and Allograft Injury
Session Type: Concurrent Session
Date: Tuesday, May 5, 2015
Session Time: 2:15pm-3:45pm
 Presentation Time: 3:15pm-3:27pm
Presentation Time: 3:15pm-3:27pm
Location: Room 118-AB
We studied the effect of time post-transplant on atrophy-fibrosis (AF) and the molecular associations with AF in 703 kidney transplant indication biopsies (bx) 3 days to 35 years post-transplant. The number of bx with fibrosis increased strikingly with time post-transplant, yet 50% of bx >1yr still had minimal AF (ci≤1). Most bx with AF (ci>1) (74%) were attributable to time-dependent diseases (eg. ABMR, GN, TG). Moreover, some bx called IFTA probably had diseases that were not diagnosable due to advanced AF.
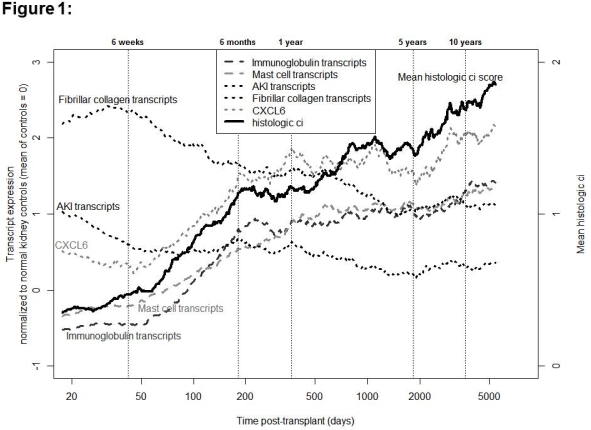
The top molecular correlates of AF were immunoglobulin and mast cell transcripts and acute kidney injury (AKI) transcripts. The top single transcript associated with AF was CXCL6. However, some of these were also strongly correlated with the time of bx post-transplant alone, particularly immunoglobulin and mast cell transcripts. When analyzed in late bx (>1yr), some molecular correlates of AF were not strongly correlated with time: AKI and fibrillar collagen transcripts and CXCL6 (Table 1). Fibrillar collagen and AKI transcript expression peaked in the first 6 weeks post-transplant when there is little AF (Figure 1), despite being associated with fibrosis in late bx. None of the transcripts associated with AF indicated uncontrolled fibrogenesis.
We conclude that AF in kidney transplant bx is not due to independent progressive fibrosis but rather the cumulative effect of injury/disease over time. Each new cycle of injury/disease induces a complex time-dependent response to wounding, which first involves AKI and fibrillar collagen transcripts and inflammation, followed by several months of plasma cell and mast cell infiltration, and then stabilizes as uninflamed AF like any wound until new wounding occurs. AF is associated with progression-to-failure because it indicates previous injury, but the real risk is that those injuries/diseases may still be operating.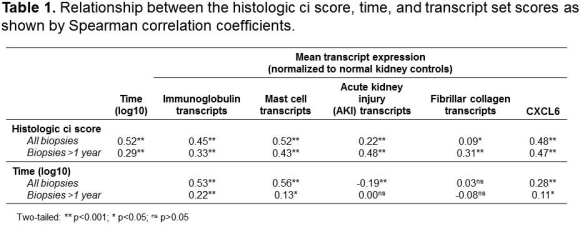
To cite this abstract in AMA style:
Venner J, Famulski K, Halloran P. Molecular Correlates of Atrophy-Fibrosis in Human Kidney Transplants Provides a New Model of Renal Fibrosis [abstract]. Am J Transplant. 2015; 15 (suppl 3). https://atcmeetingabstracts.com/abstract/molecular-correlates-of-atrophy-fibrosis-in-human-kidney-transplants-provides-a-new-model-of-renal-fibrosis/. Accessed March 1, 2026.« Back to 2015 American Transplant Congress
