Establishment of Spontaneous Tolerance of Kidney Allografts is Dependent on Mitigation of Ischemia-Reperfusion Injury via the BLTA-HVEM Pathway
1Massachusetts General Hospital, Boston, MA, 2La Jolla Institute for Allergy & Immunology, La Jolla, CA
Meeting: 2020 American Transplant Congress
Abstract number: A-368
Keywords: Graft failure, Renal injury, Renal ischemia, Tolerance
Session Information
Session Name: Poster Session A: Ischemia Reperfusion & Organ Rehabilitation
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Kidney allografts transplanted across certain mouse strain combinations (e.g. DBA/2 to B6) develop tolerance while other combinations do not (e.g. B6 to DBA/2). We have recently shown that DBA/2 plasmacytoid dendritic cells (pDCs) are more potent in inducing Foxp3+ in B6 T cells in vitro than the reverse combination, which correlates with survival of the kidney allografts. We have now shown that resident pDCs from DBA/2 kidneys are distinct from resident B6 renal pDCs in that there is a subpopulation of BTLA+ (B- and T-lymphocyte attenuator+) DBA/2 renal pDCs which are absent in B6 renal pDCs.
*Methods: BTLA is a ligand for tumor necrosis factor receptor superfamily member 14 (TNFRSF14), also known as herpes virus entry mediator (HVEM). In this study, we test what the significance of BTLA positivity may be by using B6.HVEM KO recipients.
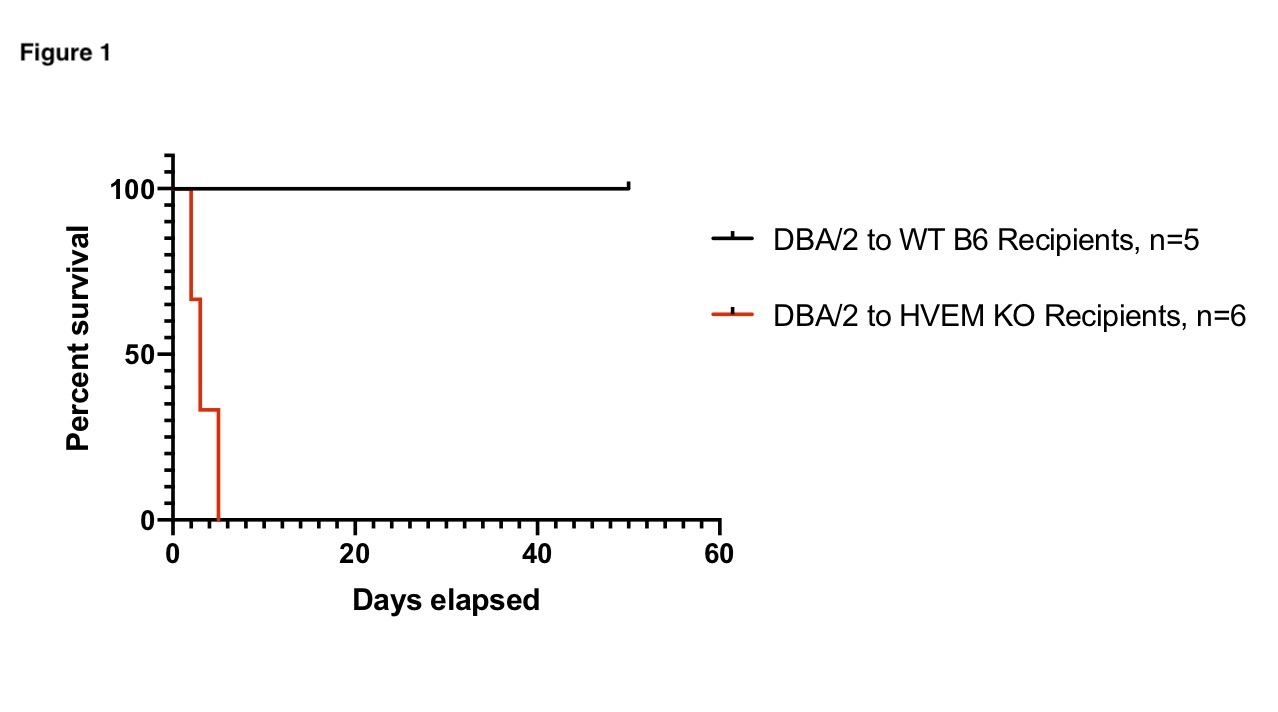
*Results: Transplantation of DBA/2J kidneys into B6.HVEM KO recipients resulted in a median survival of 3 days post-transplant (Figure 1). In contrast,when DBA/2 kidney allografts where transplanted into B6 WT recipients, spontaneous acceptance was observed (Figure 1). Pathological analyses of sample tissue from kidney allografts recovered from B6.HVEM KO recipients show severe ischemia-reperfusion injury (IRI) (Figure 2). Similar survival curves and IRI was observed in syngeneic renal transplants when using B6.HVEM KO recipients, suggesting that massive IRI cannot be overcome following transplantation into mouse recipients lacking HVEM. Nanostring analyses of IRI renal allograft samples show that the top 10 expressed genes, which include osteopontin, lamp1, urokinase, clusterin, lcn2 (NGAL), are distinct from the top genes expressed in a rejecting or tolerant kidney allograft.
*Conclusions: The BTLA-HVEM pathway is known to be co-inhibitory with regards to an immune response. Macrophages and neutrophils, which contribute to IRI, express high levels of HVEM. We postulate that kidney allografts that have resident BTLA+ pDCs regulate macrophage and neutrophil function via the BTLA-HVEM pathway and this contributes to the mitigation of IRI, allowing allo-kidneys that have the potential of inducing spontaneous acceptance to proceed with the eventual induction of tolerance.
To cite this abstract in AMA style:
Yuan Q, Hong S, Szuter E, Zhao Y, Acheampong E, Rosales I, Kronenberg M, Russell P, Madsen J, Colvin R, Alessandrini A. Establishment of Spontaneous Tolerance of Kidney Allografts is Dependent on Mitigation of Ischemia-Reperfusion Injury via the BLTA-HVEM Pathway [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/establishment-of-spontaneous-tolerance-of-kidney-allografts-is-dependent-on-mitigation-of-ischemia-reperfusion-injury-via-the-blta-hvem-pathway/. Accessed February 23, 2026.« Back to 2020 American Transplant Congress