Development of Post-Transplant DSA Following Immunosuppression Minimization/Withdrawal in Liver Transplant Recipients
1Terasaki Research Institute, Los Angeles
2University of Pennsylvania, Philadelphia, PA
3Immune Tolerance Network, Seattle, WA.
Meeting: 2018 American Transplant Congress
Abstract number: 591
Keywords: HLA antibodies, Liver transplantation, Tolerance
Session Information
Session Name: Concurrent Session: Tolerance: Clinical Studies
Session Type: Concurrent Session
Date: Tuesday, June 5, 2018
Session Time: 4:30pm-6:00pm
 Presentation Time: 5:42pm-5:54pm
Presentation Time: 5:42pm-5:54pm
Location: Room 210
Despite the allograft-risk associated with DSA, the development of post-transplant HLA donor-specific antibody (DSA) is not well described in liver transplant (LT) patients undergoing immunosuppression (IS) minimization and IS withdrawal.
We analyzed the post-transplant DSA development, defined as the development of de novo DSA (dnDSA) or the rebound of pre-transplant DSA or both, in: 69 LT patients, enrolled in the A-WISH trial, who received calcineurin inhibitors monotherapy; and of which 40 stable patients who were randomized to IS maintenance (n=9) or IS withdrawal (n=31). Among the latter, 9 tolerant patients were off IS completely. All DSA were screened using Luminex Single antigen beads with a 1000 MFI cutoff for positivity.
Among the patients who achieved stable IS monotherapy (Figure A), the incidence of post-transplant DSA, dnDSA and pre-transplant DSA rebound was 28%, 19% and 9%, respectively. The incidence of dnDSA was higher in non-randomized patients (p=0.002). The majority of dnDSA was HLA-DQ DSA. Last, early acute rejection was associated with an increased risk of developing dnDSA (HR=13.5, 95%CI[4.03-45.22]).
Among the stable randomized patients (Figure B), the incidence of post-transplant DSA was 65%, dnDSA was 60%, and pre-transplant DSA rebound was 13%. The incidence of dnDSA between the IS maintenance, tolerant and non-tolerant patients was similar. The majority of dnDSA was HLA-DQ DSA. Lastly, post-transplant DSA was found to be a risk factor for graft rejection during IS withdrawal (HR=6.99, 95%CI[2.64-18.54]).
In conclusion, the development of post-transplant DSA increases after an episode of early acute rejection, after early minimization of IS, and after complete withdrawal of IS. It is yet to be explored whether early expression of DSA in the setting of low or no IS is associated with long term impact on the allograft.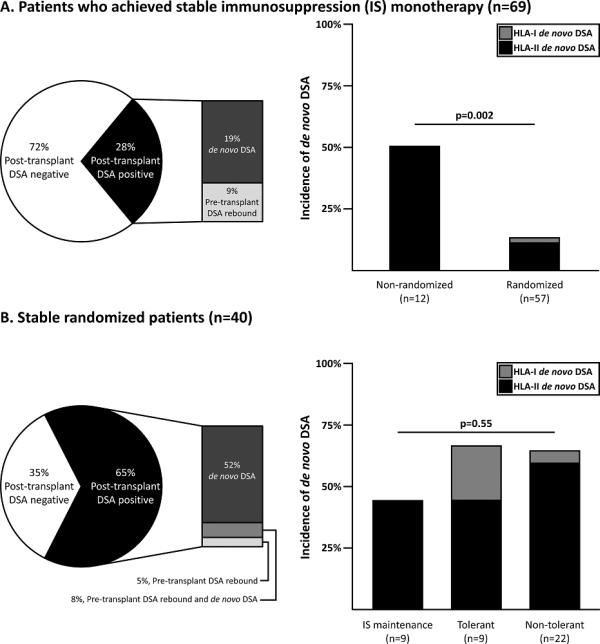
CITATION INFORMATION: Jucaud V., Shaked A., DesMarais M., Sayre P., Everly M. Development of Post-Transplant DSA Following Immunosuppression Minimization/Withdrawal in Liver Transplant Recipients Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Jucaud V, Shaked A, DesMarais M, Sayre P, Everly M. Development of Post-Transplant DSA Following Immunosuppression Minimization/Withdrawal in Liver Transplant Recipients [abstract]. https://atcmeetingabstracts.com/abstract/development-of-post-transplant-dsa-following-immunosuppression-minimization-withdrawal-in-liver-transplant-recipients/. Accessed July 18, 2025.« Back to 2018 American Transplant Congress
