DCD Utilization in Cholestatic Liver Disease: Distinct Outcomes between PSC and PBC Recipients
Abdominal Transplant Surgery, Oregon Health & Science University, Portland, OR.
Meeting: 2018 American Transplant Congress
Abstract number: A278
Keywords: Bile duct, Donors, Liver transplantation, non-heart-beating, Primary sclerosing cholangitis
Session Information
Session Name: Poster Session A: Liver: MELD, Allocation and Donor Issues (DCD/ECD)
Session Type: Poster Session
Date: Saturday, June 2, 2018
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Hall 4EF
Background: Concern for inferior outcomes in patients with primary sclerosing cholangitis (PSC) and primary biliary cholangitis (PBC) have limited utilization of donation after cardiac death (DCD) livers in these patients. Previous reports suggest inferior outcomes for PSC recipients of DCD livers and scant data exist for PBC. The aim of this study was to compare DCD graft survival for PSC/PBC patients to recipients with other etiologies of liver disease.
Methods: The UNOS database (2002-16) was used to select patients who received DCD donor liver. Demographic data for donors and recipients were analyzed. Exclusion criteria included: age <18, split grafts, cold ischemia >16 hrs, re-transplantation, and multi-organ transplant. Unadjusted graft survival was determined using the Kaplan Meier log-rank method. Predictors of graft failure were modeled using Cox regression. A p-value of < 0.05 was significant.
Results: A total of 3,258 patients received grafts from DCD donors, 91 had PBC and 125 had PSC. Compared to the recipient cohort for brain death donors, PSC and PBC recipients received proportionally fewer DCD organs (8.2% in DBD vs. 6.6% in DCD, p<0.01). For all DCD grafts, unadjusted graft survival was not different for PSC patients compared to other recipients (p=0.38); whereas PBC recipients had improved survival (p=0.01, Figure). On multivariate analysis, PSC was not a predictor of graft failure (HR 1.02, 95% CI 0.73-1.43) while PBC predicted a lower hazard of graft failure (HR 0.6, 95% CI 0.37-0.96). Additional predictors of graft failure included donor age, cold ischemia time, cause of donor death, MELD score, and recipient diabetes.
Conclusions:This study demonstrates continued bias against utilizing DCD liver in PSC and PBC recipients. Furthermore, graft survival is not inferior for PSC patients who receive DCD livers, and may actually be better in the setting of PBC. The presence of cholestatic liver disease should not preclude utilization of DCD donors. 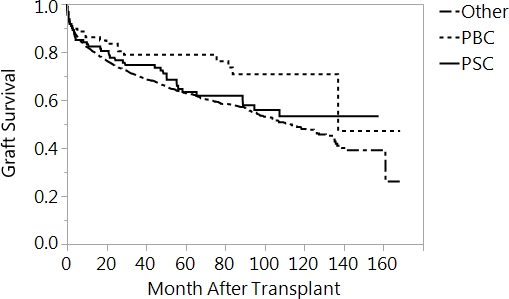
CITATION INFORMATION: Pasko J., Maynard E., Dewey E., Roayaie K., Orloff S., Scott D., Naugler W., Ahn J., Enestvedt C. DCD Utilization in Cholestatic Liver Disease: Distinct Outcomes between PSC and PBC Recipients Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Pasko J, Maynard E, Dewey E, Roayaie K, Orloff S, Scott D, Naugler W, Ahn J, Enestvedt C. DCD Utilization in Cholestatic Liver Disease: Distinct Outcomes between PSC and PBC Recipients [abstract]. https://atcmeetingabstracts.com/abstract/dcd-utilization-in-cholestatic-liver-disease-distinct-outcomes-between-psc-and-pbc-recipients/. Accessed July 18, 2025.« Back to 2018 American Transplant Congress
