Histologic Predictors of Graft Loss in Early Clinically Indicated Biopsies After Kidney Transplantation
1Einstein-Montefiore Transplant Center, Bronx, NY, 2Montefiore Medical Center, Bronx, NY, 3Transplant, Montefiore Medical Center, Bronx, NY, 4Montefiore Medical Center, New York, NY, 5Einstein-Montefiore Transplant Center, Scarsdale, NY, 6Albert Einstein College of Medicine, Montefiore Medical Ctr, Bronx, NY
Meeting: 2022 American Transplant Congress
Abstract number: 847
Keywords: Biopsy, Graft survival, Inflammation, Prognosis
Topic: Clinical Science » Kidney » 47 - Kidney Complications: Immune Mediated Late Graft Failure
Session Information
Session Name: Kidney Complications: Immune Mediated Late Graft Failure
Session Type: Poster Abstract
Date: Saturday, June 4, 2022
Session Time: 5:30pm-7:00pm
 Presentation Time: 5:30pm-7:00pm
Presentation Time: 5:30pm-7:00pm
Location: Hynes Halls C & D
*Purpose: We aimed to investigate histopathological predictors of graft lost in patients who underwent clinically indicated biopsies for worsening kidney function and/or proteinuria within 3 years after kidney transplantation to determine the effects of microvascular (MVI) and interstitial inflammation
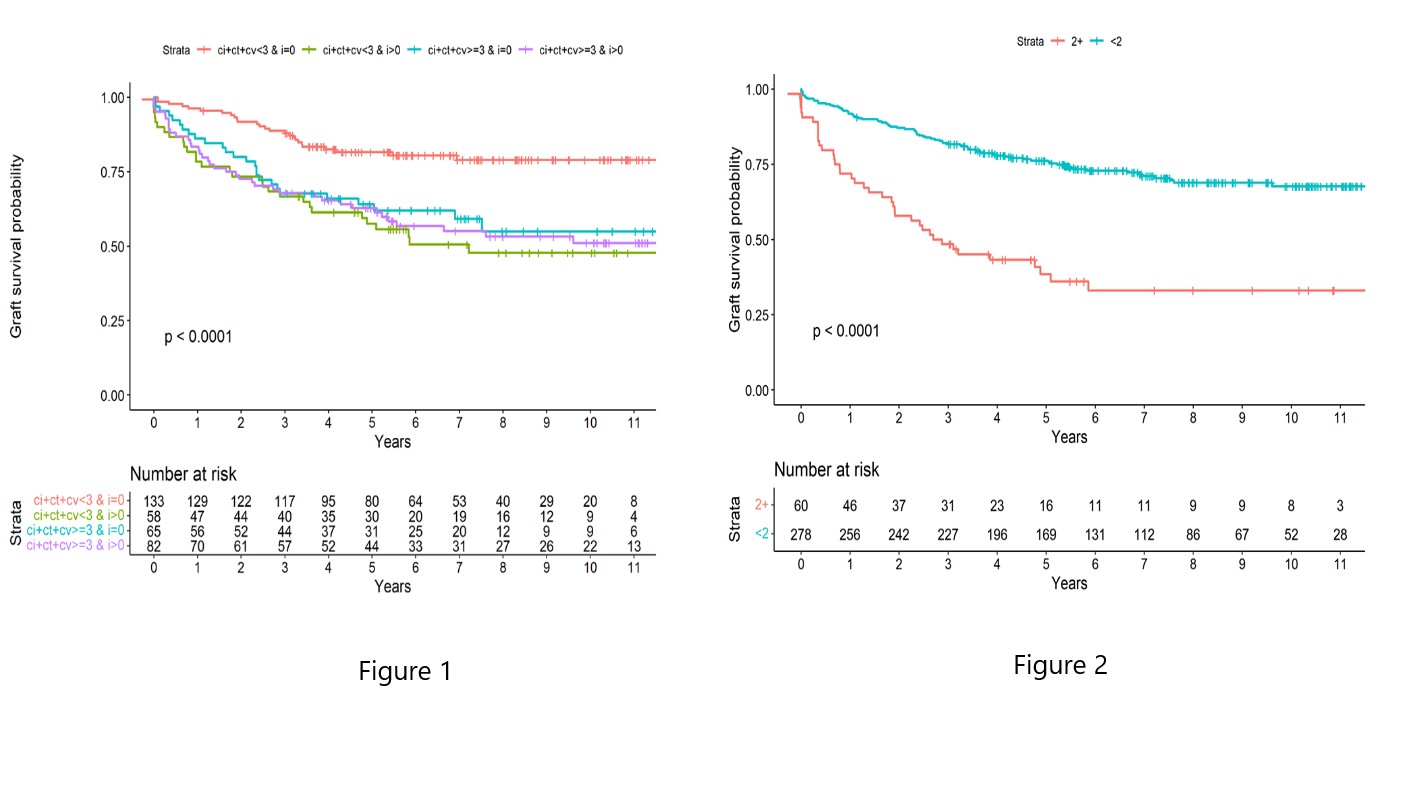
*Methods: From January 2009 till 2018, we performed a retrospective review of 343 kidney transplant patients who received a for cause kidney biopsy within 3 months to 3 years post-transplant. Acute and chronic allograft injury scores of Banff classification were used. We subgrouped the patients in terms of MVI score < 2 and ≥2 and with chronic allograft injury score (ci+ct+cv) < 3 and ≥ 3 with and without interstitial inflammation.
*Results: Transplant kidneys biopsies are done at a median of 8.8 months [IQR:4.4-21.1] after kidney transplantation. The histopathological diagnosis was as following: 13.7 % T cell mediated rejection, 9.5% antibody-mediated rejection, 6.4 % transplant glomerulopathy without donor-specific antibody, 6.4 %, recurrent/de novo glomerular disease, 4.6 % BKV nephropathy, and the rest 59.1% were normal or had non-specific interstitial fibrosis and tubular atrophy and/or acute tubular necrosis. During a median follow up of 65.9 months [IQR:36.7-102.7] after kidney biopsy, 34.6 % recipients lost their allograft. In univariate analysis, the following factors were significant for graft loss: African American race (P=0.001), creatinine at the time of biopsy (p<0.001), spot urine to creatinine ratio(UPC) at the time of biopsy (p=0.001), class I and II DSA> 5000 MFI at the time of biopsy (p<0.001), previous rejection (p=0.001), ci+ct+cv <3 and i >0 (p=0.001), ci+ct+cv>3 and = 0 (p=0.002), ci+ct+cv>3 and i>0 (p<0.001), and MVI >2 (p<0.001)[Fig 1]. Kaplan-Meier survival curve showed significantly lower allograft survival in patients with MVI score > 2 (p < 0.0001) and chronic allograft injury score ≥ 3 with or without inflammation or chronic allograft injury score < 3 with inflammation as compared to chronic allograft injury score < 3 (p < 0.0001) [Fig 2].
*Conclusions: Interstitial inflammation and microvascular inflammation observed in early transplant kidney biopsies are associated for lower allograft survival
To cite this abstract in AMA style:
Ajaimy M, Hemmige V, Liriano-Ward LE, Azzi Y, Kapoor S, Loarte P, Pynadath C, Colovai A, Akalin E. Histologic Predictors of Graft Loss in Early Clinically Indicated Biopsies After Kidney Transplantation [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/histologic-predictors-of-graft-loss-in-early-clinically-indicated-biopsies-after-kidney-transplantation/. Accessed February 18, 2026.« Back to 2022 American Transplant Congress