Nuclear Co-Repressor Complex Inhibition Reverses Benefit of HDAC2 Deletion in Renal Ischemia.
1Surgery, University of Pennsylvania, Philadelphia, PA
2Pathology, University of Pennsylvania, Philadelphia, PA
3Pathology, Children's Hospital of Philadelphia, Philadelphia, PA
4Pharmacology and Molecular Sciences, Johns Hopkins University, Baltimore, MD
5Surgery, Children's Hospital of Philadelphia, Philadelphia, PA
Meeting: 2017 American Transplant Congress
Abstract number: B129
Keywords: Graft function, Renal injury, Renal ischemia, Warm ischemia
Session Information
Session Name: Poster Session B: Ischemic Injury and Organ Preservation Session II
Session Type: Poster Session
Date: Sunday, April 30, 2017
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall D1
Introduction: Class I histone/protein deacetylases (HDACs) 1 and 2 bear >85% protein sequence homology and conventionally are thought to have similar function via occupancy in nuclear co-repressor complexes. Class I HDAC inhibition has been shown to mitigate renal warm ischemia-reperfusion injury (IRI) in mice.
Methods: Wild type C57BL/6 (WT) and whole animal-inducible HDAC1- or 2- gene deleted mice (HDAC1-/- or HDAC2-/-) were subjected to standardized warm renal IRI consisting of unilateral clamping of the renal pedicle and contralateral nephrectomy. Primary renal tubular epithelial cell (RTEC) cultures were derived from each genetic strain for protein analysis.
Results: HDAC1-/- mice have impaired IRI tolerance compared to B6 controls (p<0.01, Fig 1a) whereas HDAC2-/- mice demonstrate profound protection from renal IRI (p<0.01, Fig 1b). Protein analysis from RTEC nuclear extracts shows that deletion of either HDAC1 or 2 is associated with compensatory enhanced protein expression of the other. Pulldown experiments demonstrate that HDAC2 deletion leads to enhanced HDAC1 association with the CoREST nuclear co-repressor complexes and increased protein expression of co-repressor components. In vivo inhibition of the CoREST complex in both WT and HDAC2-/- mice increased vulnerability to renal IRI injury and returned HDAC2-/- mice to a WT renal IRI phenotype (Fig 1c).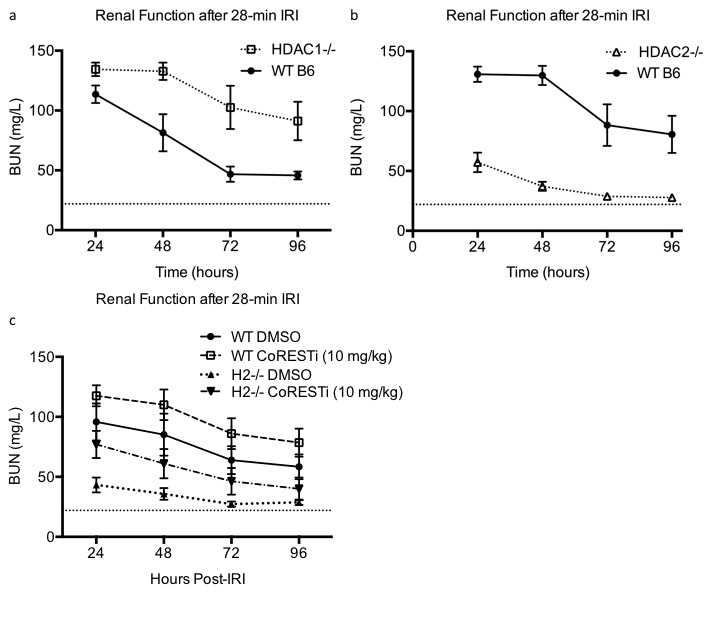 Conclusion: HDAC1 and 2 have reciprocal effects on murine renal IRI tolerance, with HDAC1 deletion increasing vulnerability and HDAC2 deletion providing substantial protection from warm and cold ischemia. HDAC2 deletion leads to alteration in expression and likely stability of nuclear co-repressor complexes, and its effect can be reversed with inhibition of the CoREST complex.
Conclusion: HDAC1 and 2 have reciprocal effects on murine renal IRI tolerance, with HDAC1 deletion increasing vulnerability and HDAC2 deletion providing substantial protection from warm and cold ischemia. HDAC2 deletion leads to alteration in expression and likely stability of nuclear co-repressor complexes, and its effect can be reversed with inhibition of the CoREST complex.
CITATION INFORMATION: Aufhauser Jr D, Murken D, Wang Z, Samanta A, Ge G, Bhatti T, Cole P, Kalin J, Hancock W, Levine M. Nuclear Co-Repressor Complex Inhibition Reverses Benefit of HDAC2 Deletion in Renal Ischemia. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Jr DAufhauser, Murken D, Wang Z, Samanta A, Ge G, Bhatti T, Cole P, Kalin J, Hancock W, Levine M. Nuclear Co-Repressor Complex Inhibition Reverses Benefit of HDAC2 Deletion in Renal Ischemia. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/nuclear-co-repressor-complex-inhibition-reverses-benefit-of-hdac2-deletion-in-renal-ischemia/. Accessed January 21, 2026.« Back to 2017 American Transplant Congress
