Risk of Ischemic Biliary Injury Is Not Associated with Prolonged Hepatic Artery Ischemic Times During Liver Transplantation.
1Univ. Colorado, Aurora, CO
2Univ. Washington, Seattle, WA
Meeting: 2017 American Transplant Congress
Abstract number: 250
Keywords: Bile duct, Graft failure, Ischemia, Liver transplantation
Session Information
Session Name: Concurrent Session: Liver Retransplantation and Other Complications
Session Type: Concurrent Session
Date: Monday, May 1, 2017
Session Time: 2:30pm-4:00pm
 Presentation Time: 3:06pm-3:18pm
Presentation Time: 3:06pm-3:18pm
Location: E353B
Biliary strictures after liver transplant (LT) are associated with increased patient morbidity and graft failure. AIM: To assess the association of duration of hepatic artery ischemic time (time from portal vein to hepatic artery anastomosis) and post-LT biliary strictures. METHODS: In a large retrospective study of 804 LT recipients from 2008-14, we assessed recipient (age, gender, liver disease, MELD at LT), donor (age, cause of death, circulatory vs brain death, donor type, cold ischemic time) and operative factors (warm ischemic time (WIT), hepatic artery ischemic time (AIT), total ischemic time (TIT)). Patients with hepatic artery thrombosis were excluded. Post-LT biliary strictures were rigorously assessed by detailed chart review and categorized as diffuse ischemic type biliary injury or >2 non-anastomotic strictures, non-anastomotic strictures or anastomotic strictures. Logistic regression was performed. RESULTS: Of the 804 LT recipients, 550 (68%) were male with median (IQR) age at LT 55 (47-59) years, MELD at LT 28 (23-31), donor age 33 (22-47), and 41 (5%) donation after circulatory death. The median (IQR) WIT was 36 min (29-45), AIT 37 min (28-50), TIT 74 min (61-88). Quartile cut offs for AIT in min were: ≤28, >28-37, >37-50, >50. After LT, 48 (6%) had diffuse structuring or >2 non-anastomotic strictures, 58 (7%) had non-anastomotic strictures and 145 (18%) had anastomotic strictures. Using quartiles of AIT, multiple variable logistic regression models controlling for recipient and donor factors demonstrated no significant increase in risk of diffuse ischemic type biliary injury or non-anastomotic biliary strictures or anastomotic biliary strictures, with increasing hepatic artery ischemic time. CONCLUSION: Arterial Ischemic Time (time from portal vein to hepatic artery anastomosis) appears not to have a strong association with diffuse biliary ischemic time injury or multiple non-anastomotic biliary stricture. Meticulous attention to hepatic artery anastomosis during LT is needed, even if it increases time taken. 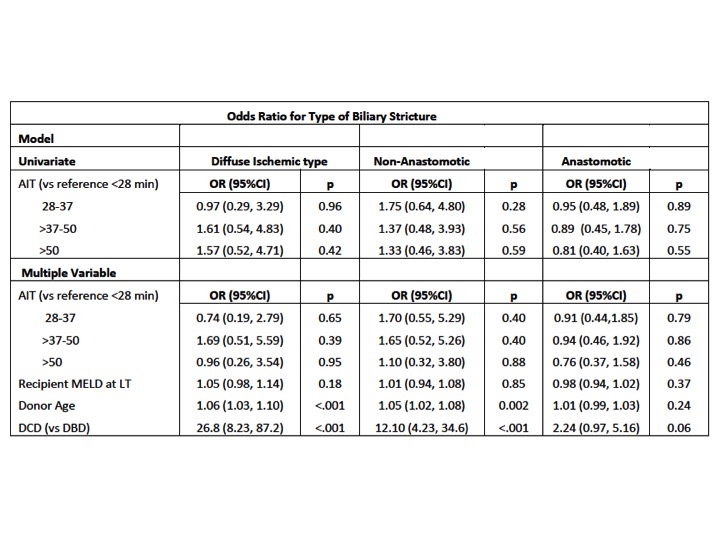
CITATION INFORMATION: Armenia E, Schomaker N, Kalra A, Gralla J, Truesdale A, Biggins S, Nydam T, Burton J. Risk of Ischemic Biliary Injury Is Not Associated with Prolonged Hepatic Artery Ischemic Times During Liver Transplantation. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Armenia E, Schomaker N, Kalra A, Gralla J, Truesdale A, Biggins S, Nydam T, Burton J. Risk of Ischemic Biliary Injury Is Not Associated with Prolonged Hepatic Artery Ischemic Times During Liver Transplantation. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/risk-of-ischemic-biliary-injury-is-not-associated-with-prolonged-hepatic-artery-ischemic-times-during-liver-transplantation/. Accessed February 19, 2026.« Back to 2017 American Transplant Congress
