Anti-LG3 Antibodies Aggravate Ischemia-Reperfusion Injury
1Centre de Recherche du Centre Hospitalier de l'Université
de Montréal (CRCHUM) and Université
de Montréal, Montréal, Canada
2Department of Pathology, CHU Ste-Justine Université
de Montréal, Montréal, Canada.
Meeting: 2015 American Transplant Congress
Abstract number: C17
Keywords: Apoptosis, Endothelial cells, Graft acceptance, Renal ischemia
Session Information
Session Name: Poster Session C: Antigen Presenting Cells in Alloimmune Responses/B Cells and Antibody in Alloimmune Responses
Session Type: Poster Session
Date: Monday, May 4, 2015
Session Time: 5:30pm-6:30pm
 Presentation Time: 5:30pm-6:30pm
Presentation Time: 5:30pm-6:30pm
Location: Exhibit Hall E
Ischemia-Reperfusion Injury (IRI) is a significant cause of renal allograft dysfunction and a risk factor for poor long-term graft outcomes. Microvascular injury is an important component of IRI. LG3, a truncated C-terminal perlecan fragment is released by apoptotic endothelial cells, renal transplant patients with anti-LG3 antibodies develop more severe forms of rejection. We demonstrated previously that the passive transfer of anti-LG3 antibodies, in an animal model of vascular rejection, aggravates vascular remodeling and C4d deposition. Here, we plan to evaluate whether anti-LG3 antibodies can enhance IRI-associated vascular damage. Unilateral renal artery clamping for 30 minutes plus contra-lateral nephrectomy was performed in C57Bl/6 mice. Intra-venous injections of anti-LG3 antibodies or mouse control IgG were performed 2 days prior to renal artery clamping and every other day thereafter. Serum and urine were collected at days 2 and 7 post-IRI, and mice were scarified at day 2 or day 7 post-surgery. Compared to the control group, mice passively transferred with anti-LG3 antibodies had higher serum BUN levels at day 2 post-IRI (p =0.0372, n= 7 per group) and a trend toward higher BUN persisted at day 7 (p=0.087, n=5 per group). Creatinine levels were significantly increased at day 7 post-IRI in anti-LG3-transferred mice (p =0.0373,n≥4 per group). IRI led to increased urinary LG3 levels. Passive anti-LG3 transfer decreased urinary LG3, suggesting the possibility of immune complex formation and intra-renal deposition. In support of this hypothesis, immunohistochemistry for C4d demonstrated increased renal C4d glomerular staining (p =0.0083, n= 5 per group) in anti-LG3 treated mice. Anti-LG3 transfer also significantly increased C4d staining in cortico-medullary peri-tubular capillaries (p =0.0022, n= 5 per group).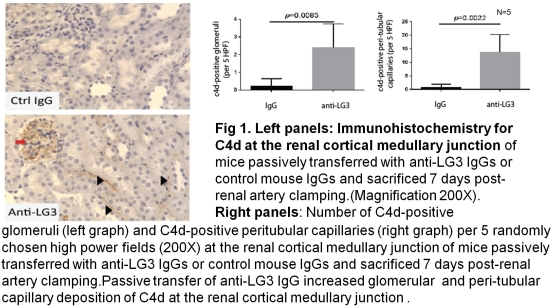 Together, our results highlight an important role for anti-LG3 antibodies in aggravation of microvascular injury and renal dysfunction during IRI.
Together, our results highlight an important role for anti-LG3 antibodies in aggravation of microvascular injury and renal dysfunction during IRI.
To cite this abstract in AMA style:
Yang B, Hamelin K, Pomerleau L, Peng J, Tremblay J, Patey N, Hébert M-J. Anti-LG3 Antibodies Aggravate Ischemia-Reperfusion Injury [abstract]. Am J Transplant. 2015; 15 (suppl 3). https://atcmeetingabstracts.com/abstract/anti-lg3-antibodies-aggravate-ischemia-reperfusion-injury/. Accessed February 12, 2026.« Back to 2015 American Transplant Congress
