Under-Diagnosed Hyperoxalosis in Transplant-Listed Patients
Nephrology, Johns Hopkins University, Baltimore, MD
Meeting: 2020 American Transplant Congress
Abstract number: B-095
Keywords: Biopsy, Graft survival, Kidney transplantation, Retransplantation
Session Information
Session Name: Poster Session B: Kidney Complications: Non-Immune Mediated Late Graft Failure
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: In an era of increasing kidney transplantation (KTx), hyperoxalosis remains an under-recognized cause for allograft failure. Bariatric interventions are significant risk factors for oxalosis, but hyperoxalosis in sleeves and other intestinal surgeries are not well characterized in end stage kidney disease (ESKD). Screening and monitoring for hyperoxalosis in KTx candidates is neither routinely done nor is screening easily accomplished. We investigated the rate of hyperoxalosis and risk factors in transplant-listed ESKD and non-ESKD patients with history of bariatric interventions. We believe that allograft failure from hyperoxalosis may be an emerging national problem.
*Methods: This is a cross-sectional study using registry data from electronic medical records at a single, large transplant institution. Patients were evaluated for KTx between 2010-2015 and measured the serum oxalate level at the time of KTx evaluation as part of their routine care. We classified patients into six categories based on etiology of hyperoxalosis. We calculated the prevalence of hyperoxalosis among these groups and compared demographics, baseline clinical characteristics, and serum oxalate level. Possion regression was used for analysis.
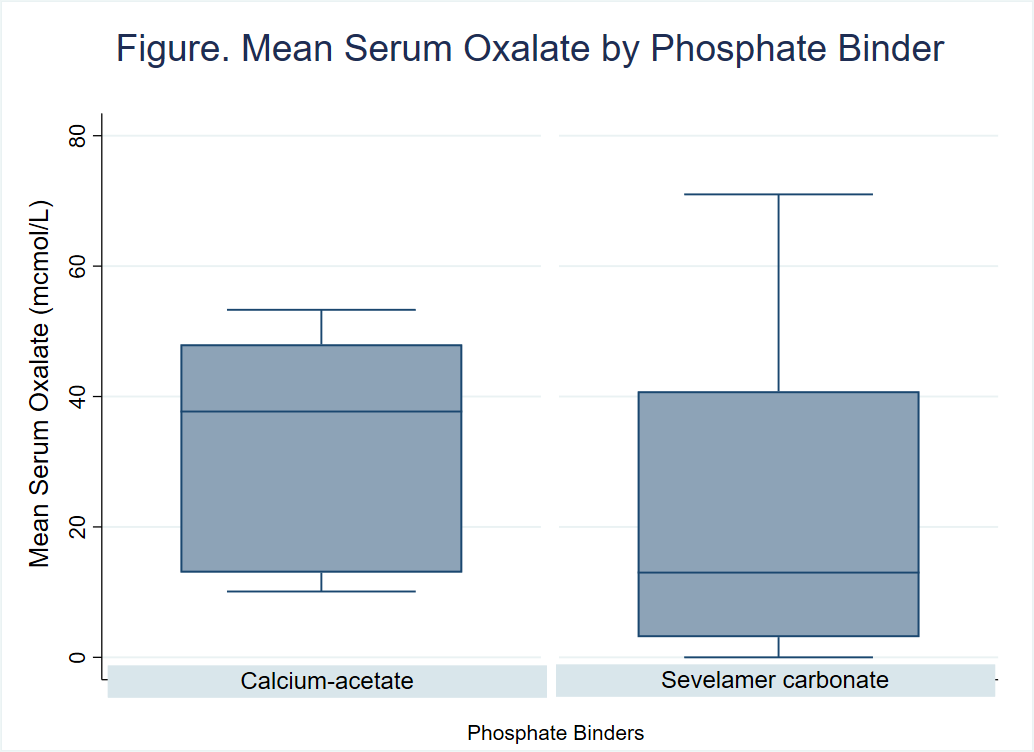
*Results: Across six risk categories, gastric bypass (n=16), sleeve (n=7), lap-band (n=3), Inflammatory Bowel Disease (n=3), colectomy/intestinal bypass (n=3), and cystic fibrosis (n=2), the prevalence of hyperoxalosis was 63%, 100%, 33%, 67%, 50%, and 67%, respectively. Age, sex, race, co-morbidities, history of prior transplantation, and dialysis modality were similar between the groups; however, BMI was significantly highest among post-sleeve gastrectomy patients (p=0.002). There was no difference in mean phosphorus and PTH levels among groups; however, mean calcium level was significantly lower in colectomy/intestinal bypass group (p=0.037). Bariatric sleeves and intestinal surgeries had the largest range of serum oxalate levels. Nephrolithiasis was reported in 100% of colectomy/intestinal bypass, 67% in cystic fibrosis, and 13% in bariatric surgeries (p=0.01). Mean serum oxalate levels were lower in patients on non-calcium-based binders as opposed to calcium-based binder (Figure). ESKD was higher in patients with hyperoxalosis. As a control, there were 3 donors at risk for oxalosis (2 with sleeve and 1 lap-band bypasses) without hyperoxalosis.
*Conclusions: ESKD patients with newer forms of bariatric interventions are at risk of hyperoxalosis and should consider screening for serum oxalate levels prior to KTx.
To cite this abstract in AMA style:
Tariq A, Lakhani L, Greenspan W, Alasfar S, Naqvi F, Brennan D. Under-Diagnosed Hyperoxalosis in Transplant-Listed Patients [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/under-diagnosed-hyperoxalosis-in-transplant-listed-patients/. Accessed July 18, 2025.« Back to 2020 American Transplant Congress