The Importance of Persistent and Recurrent T Cell Mediated Rejection in Tacrolimus Treated Renal Transplant Recipients
1Department of Medicine, University of Manitoba, Winnipeg, MB, Canada, 2Department of Pathology, University of Manitoba, Winnipeg, MB, Canada, 3Shared Health Services Manitoba, Winnipeg, MB, Canada, 4Department of Pediatrics and Child Health, University of Manitoba, Winnipeg, MB, Canada, 5Department of Pediatrics, University of British Columbia, Winnipeg, MB, Canada
Meeting: 2021 American Transplant Congress
Abstract number: LB 77
Keywords: Graft failure, HLA antibodies, Rejection, T cells
Topic: Clinical Science » Kidney » Kidney Complications: Immune Mediated Late Graft Failure
Session Information
Session Name: Kidney Complications: Immune Mediated Late Graft Failure
Session Type: Poster Abstract
Session Date & Time: None. Available on demand.
Location: Virtual
*Purpose: Optimal follow-up after treatment for T-cell mediated rejection (TCMR) is not well-established. We sought to identify the prevalence and clinical associations of repeated TCMR events.
*Methods: We retrospectively reviewed consecutive renal transplant recipients from 2001-2019 at a single-center which utilizes an early surveillance biopsy program.
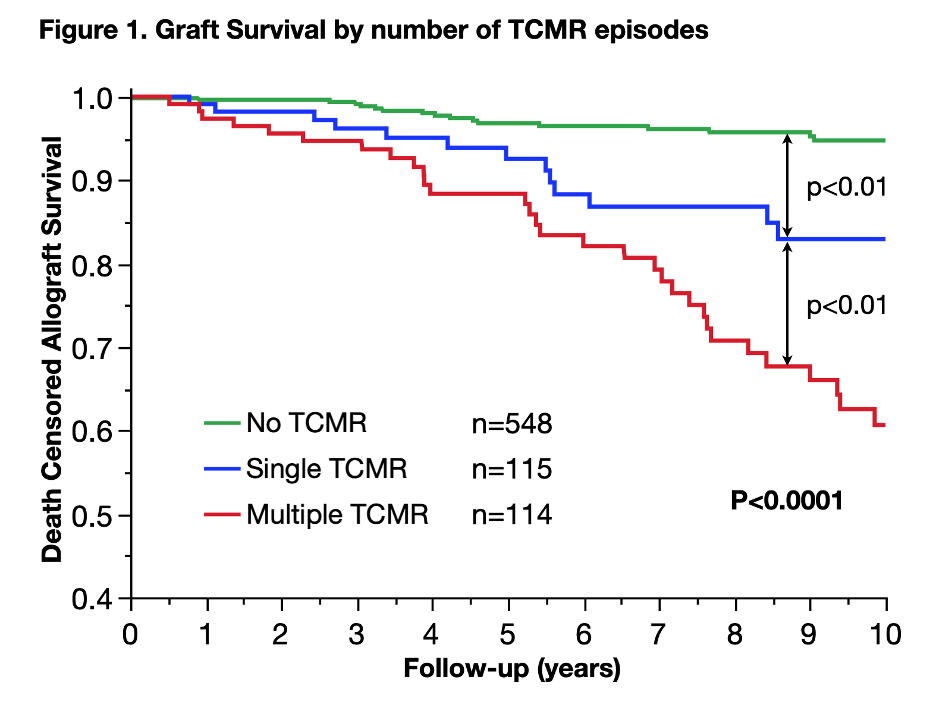
*Results: 2,083 biopsies were performed in 777 recipients and TCMR was detected in 229 recipients, with the majority (61%) being Banff borderline rejection. 179 recipients had a follow-up biopsy at a median of 3 months (IQR 1.3-8.5). Persistent TCMR was found in 50% of recipients at a median of 2.4 months (IQR 1.1-6.3 months). Recurrent TCMR after a negative follow-up biopsy was found in 14% of recipients at a median of 12 months (IQR 2.9-22.7). Subsequent follow-up biopsies revealed that after each additional TCMR event >50% of recipients had another TCMR. Repeated events correlated with HLA-DR/DQ alloimmune risk category. Recipients with persistent or recurrent TCMR had similar clinical outcomes and were analyzed together as recipients with “Multiple TCMR”. Recipients were more likely to have repeated TCMR events if they were younger, had greater coefficient of variation in tacrolimus trough levels, or had intermediate or high alloimmune risk categorized by HLA-DR/DQ single molecule eplet mismatch scores (p=0.0003). Allograft survival and dnDSA-free survival were decreased in recipients with single TCMR compared to no TCMR, and in recipients with multiple TCMR compared to either group (p<0.0001). (Figure 1) The correlation between allograft survival and TCMR episode number was also significant in the subset whose first TCMR biopsy was Banff borderline TCMR.
*Conclusions: Repeated TCMR events are common despite standard immunosuppression and correlate with dnDSA development and allograft loss. HLA molecular mismatch and recipient age at time of transplant may identify high-risk patients and help enrich patients to study novel therapies.
To cite this abstract in AMA style:
Rampersad C, Gibson IW, Rush DN, Pochinco D, Birk PE, Goldberg A, Blydt-Hansen T, Karpinski M, Shaw J, Ho J, Nickerson PW, Wiebe C. The Importance of Persistent and Recurrent T Cell Mediated Rejection in Tacrolimus Treated Renal Transplant Recipients [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/the-importance-of-persistent-and-recurrent-t-cell-mediated-rejection-in-tacrolimus-treated-renal-transplant-recipients/. Accessed February 20, 2026.« Back to 2021 American Transplant Congress