The Crucial Role of Molecular Microscope in the Interpretation of Ambiguous Lesions Such as Banff Borderline Changes and Tubulo-Interstitial Inflammation Accompanying PVAN
1Warsaw Medical University, Warsaw, Poland, 2ATAGC, University of Alberta, Edmonton AB, AB, Canada, 3Pomeranian Medical University, Szczecin, Poland
Meeting: 2019 American Transplant Congress
Abstract number: C172
Keywords: Biopsy, Inflammation, Kidney transplantation, Polyma virus
Session Information
Session Name: Poster Session C: Kidney: Acute Cellular Rejection
Session Type: Poster Session
Date: Monday, June 3, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall C & D
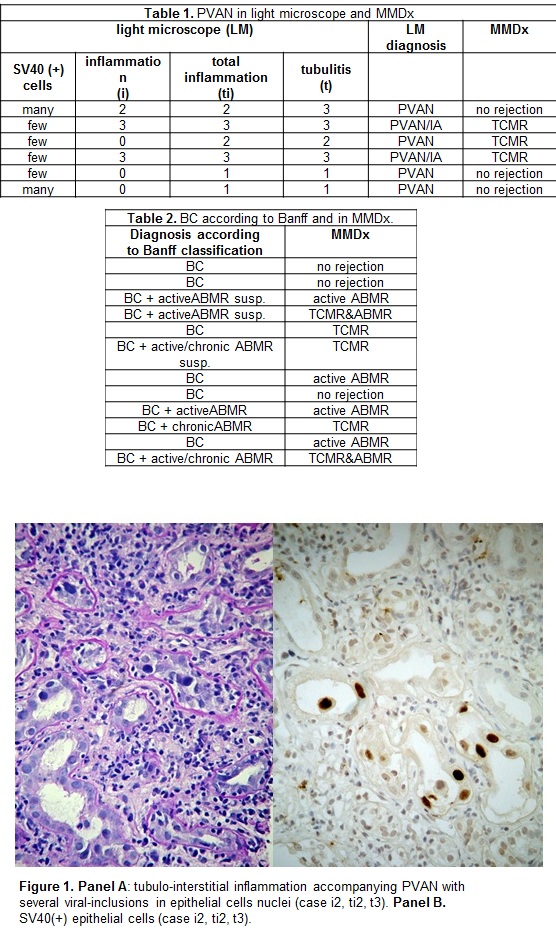
*Purpose: Anti-rejection treatment implementation is highly dependent on morphologic lesions interpretation based on Banff classification. Unfortunately, some light microscopic phenotypes are ambiguous which constricts the therapeutic decisions. Conventional microscopy does not allow for reliable recognition/ exclusion of TCMR in cases of Banff borderline changes (BC) nor in Polyomavirus-associated nephropathy (PVAN) accompanied by tubulo-interstitial inflammation (Figure 1).
*Methods: As a part of the multicenter study “Troubled Polish Kidney Transplants Biopsy” we analyzed the molecular phenotype (Molecular Microscope Diagnostic System (MMDx)) of all cases diagnosed as PVAN or as BC by conventional microscopy.
*Results: Among 90 biopsies studied in both conventional and molecular microscopes there were 6 PVAN cases and 12 biopsies with BC. In 3 (50%) of PVAN cases molecular phenotyping revealed TCMR (Table 1).There were two PVAN/IA cases that showed TCMR phenotype in MMDx, and one case diagnosed as pure BKVN by light, but as TCMR by Molecular Microscope. The cases with “no rejection” by MMDx had also “no rejection” phenotype in light microscopy. Clinical observation confirmed MMDx diagnosis in all analyzed cases of PVAN.
MMDx showed diversified molecular phenotype of BC cases (Table 2). 5 (56%) BC cases had molecular phenotype of TCMR. 6 BC cases additionally fulfilled Banff criteria for ABMR, which was confirmed by MMDx in 4 of these cases. Among 5 BC lesions not accompanied by other histological signs of rejection 3 had “no rejection” phenotype in MMDx, and 2 were identified as ABMR.
*Conclusions: Molecular Microscope may allow for the ultimate diagnosis in such ambiguous cases of tubulo-interstitial inflammation as in PVAN and Banff borderline changes. As it was confirmed by patients follow-up MMDx allows for the differentiation between pure PVAN and PVAN+TCMR. BC has diversified molecular phenotype. MMDx may have a crucial role in proper classification of BC cases.
To cite this abstract in AMA style:
Deborska-Materkowska D, Perkowska-Ptasinska A, Ciszek M, Halloran PF, Myslak M. The Crucial Role of Molecular Microscope in the Interpretation of Ambiguous Lesions Such as Banff Borderline Changes and Tubulo-Interstitial Inflammation Accompanying PVAN [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/the-crucial-role-of-molecular-microscope-in-the-interpretation-of-ambiguous-lesions-such-as-banff-borderline-changes-and-tubulo-interstitial-inflammation-accompanying-pvan/. Accessed February 18, 2026.« Back to 2019 American Transplant Congress