T Cell Exhaustion in Kidney Transplant Patients
1Department of Neurology, Icahn School of Medicine, New York
2Department of Medicine, Icahn School of Medicine, New York
3Immune Tolerance Network, Bethesda.
Meeting: 2018 American Transplant Congress
Abstract number: 403
Keywords: Induction therapy, Kidney transplantation, T cells
Session Information
Session Name: Concurrent Session: Biomarkers, Immune Monitoring and Outcomes: Basic
Session Type: Concurrent Session
Date: Tuesday, June 5, 2018
Session Time: 2:30pm-4:00pm
 Presentation Time: 2:30pm-2:42pm
Presentation Time: 2:30pm-2:42pm
Location: Room 602/603/604
Background: T cell exhaustion is a dysfunctional state that arises during chronic infection and cancer in response to persistence of high antigenic load. Whether chronic exposure to graft alloantigens leads to the formation of exhausted T cells (Tex) and, if so, whether Tex is related to graft outcome in human kidney transplant recipients is unknown.
Methods: We used mass cytometry (CyTOF) to analyze exhaustion phenotypes of serially collected PBMC from 26 kidney transplant recipients enrolled in the prospective, observational, CTOT-01 cohort (samples were obtained at month 0, 3, and 6 after transplant). Using a panel of 36 markers and unbiased clustering algorithms (Phenograph) we extracted the frequencies of 5 CD4+ and 2 CD8+ T cell subsets expressing different combination of exhaustion markers (Figure 1A).
Results: We observed significant increases in the percentages of circulating CD4+ Tex and CD8+ Tex from month 0 to month 6 in patients given induction therapy with anti-thymocyte globulin (ATG) compared to those given basiliximab or no induction (Figure 1B-C). 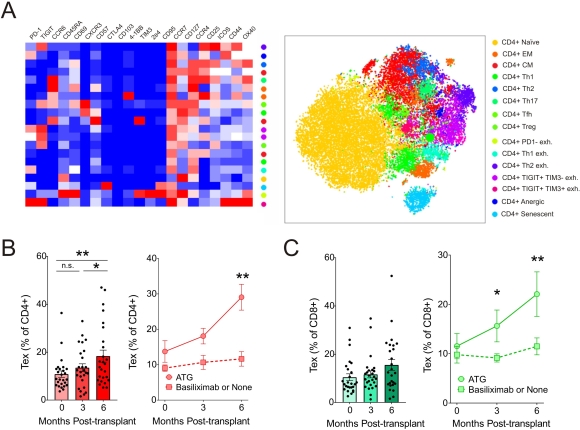 Within the Tex cells, the subsets of CD4+TIGIT+TIM3-2b4- and CD8+TIGIT+2b4+41BB-TIM3- were the most differentially increased between the two induction strategies. Percentages of CD8+TIGIT+2b4+41BB-TIM3- at 6 months correlated inversely with increasing interstitial fibrosis between 0 and 6 month surveillance graft biopsies (r:-0.54; p=0.05).
Within the Tex cells, the subsets of CD4+TIGIT+TIM3-2b4- and CD8+TIGIT+2b4+41BB-TIM3- were the most differentially increased between the two induction strategies. Percentages of CD8+TIGIT+2b4+41BB-TIM3- at 6 months correlated inversely with increasing interstitial fibrosis between 0 and 6 month surveillance graft biopsies (r:-0.54; p=0.05).
Discussion: Our findings identify previously unrecognized relationships among peripheral blood T cell exhaustion phenotypes, progressive kidney allograft injury and ATG induction and raise the possibility that these observations are mechanistically linked.
CITATION INFORMATION: Fribourg M., Fischman C., Anderson L., Burrell B., Heeger P., Cravedi P. T Cell Exhaustion in Kidney Transplant Patients Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Fribourg M, Fischman C, Anderson L, Burrell B, Heeger P, Cravedi P. T Cell Exhaustion in Kidney Transplant Patients [abstract]. https://atcmeetingabstracts.com/abstract/t-cell-exhaustion-in-kidney-transplant-patients/. Accessed July 14, 2025.« Back to 2018 American Transplant Congress
