Standard Induction Immunosuppression Interferes with the Role of Vascularized Bone Marrow in Vascularized Composite Allograft Protection
Department of Surgery, University of Maryland School of Medicine, Baltimore, MD.
Meeting: 2018 American Transplant Congress
Abstract number: A418
Keywords: Graft failure, Graft survival, Thymocytes
Session Information
Session Name: Poster Session A: Tolerance / Immune Deviation
Session Type: Poster Session
Date: Saturday, June 2, 2018
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Hall 4EF
Purpose:
Clinical induction therapies have been demonstrated to interfere with the development of immunologic tolerance in experimental models. Vascularized bone marrow (VBM) has been demonstrated to provide immunologic protection to vascularized composite allografts (VCA). We utilized a non-human primate (NHP) model of facial transplantation to investigate the effects of recipient T cell depletion and steroid therapy on VBM-mediated graft protection.
Methods:
We utilized a well-established model of heterotopic facial subunit VCA in a NHP model. Recipients (N=3) were administered 50 mg/kg of anti-thymocyte globulin (ATGAM) on Day -2, -1, and 0 and transplanted Day 0. Steroids were administered with an initial 20 mg/kg dose and tapered over 21 days and maintained on tacrolimus (Tac) and mycophenylate mofetil (MMF). Chimerism was determined using flow cytometry from peripheral blood samples and final tissues. Comparison was made to historical cohorts, VCA + VBM (n=4) and VCA (no VBM, n=3) treated with Tac/MMF.
Results:
Mean survival in the ATGAM with steroid taper group was 28.3±8.02 days, as compared to the VCA + VBM group 348.2±85.9 days, and the VCA group (no VBM) 24.7±16.6 days (p=0.008). 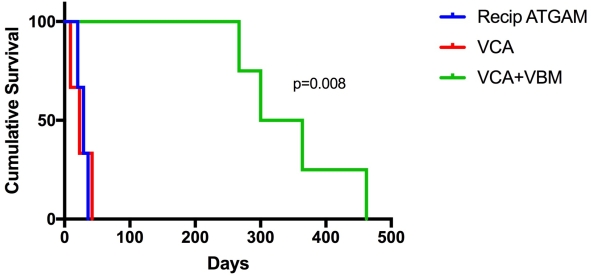 NHP receiving induction therapies developed early Banff 4 rejection, as well as histopathologic evidence of thrombophlebitis and muscle necrosis. In contrast to the VCA + VBM group, chimerism was undetected in peripheral blood and graft bone marrow was nearly acellular, with an average of 91.5%±2.4 (range 89.8-93.2%) of the lymphocytes present recipient in origin (n=2). Also in contrast to VCA + VBM but comparable to VCA (no VBM), the development of IgM and IgG donor specific antibodies was noted in the ATGAM with steroid taper group, with a mean of 357.5 and 180.5 MFI respectively.
NHP receiving induction therapies developed early Banff 4 rejection, as well as histopathologic evidence of thrombophlebitis and muscle necrosis. In contrast to the VCA + VBM group, chimerism was undetected in peripheral blood and graft bone marrow was nearly acellular, with an average of 91.5%±2.4 (range 89.8-93.2%) of the lymphocytes present recipient in origin (n=2). Also in contrast to VCA + VBM but comparable to VCA (no VBM), the development of IgM and IgG donor specific antibodies was noted in the ATGAM with steroid taper group, with a mean of 357.5 and 180.5 MFI respectively.
Conclusions:
Presumptive VBM cell populations that regulate immune responses are susceptible to T cell depleting and steroid therapies. The observed interference of standard induction therapies on the protective value of VBM highlights relationships between pharmacologic and biologic mechanisms of VCA graft protection.
CITATION INFORMATION: Shockcor N., Buckingham E., Hassanein W., Nam A., Bartlett S., Barth R. Standard Induction Immunosuppression Interferes with the Role of Vascularized Bone Marrow in Vascularized Composite Allograft Protection Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Shockcor N, Buckingham E, Hassanein W, Nam A, Bartlett S, Barth R. Standard Induction Immunosuppression Interferes with the Role of Vascularized Bone Marrow in Vascularized Composite Allograft Protection [abstract]. https://atcmeetingabstracts.com/abstract/standard-induction-immunosuppression-interferes-with-the-role-of-vascularized-bone-marrow-in-vascularized-composite-allograft-protection/. Accessed July 12, 2025.« Back to 2018 American Transplant Congress
