Should We Worry About Covid-19 Infection in Pediatric SOT?
1Surgery, Medstar Georgetown Transplant Institute, Washington, DC, 2Pediatrics, Medstar Georgetown University Hospital, Washington, DC, 3Pathology and Laboratory Medicine, Medstar Georgetown University Hospital, Washington, DC
Meeting: 2021 American Transplant Congress
Abstract number: 638
Keywords: Infection, Intestinal transplantation, Liver transplantation, Pediatric
Topic: Clinical Science » Biomarkers, Immune Assessment and Clinical Outcomes
Session Information
Session Name: Biomarkers, Immune Assessment and Clinical Outcomes
Session Type: Poster Abstract
Session Date & Time: None. Available on demand.
Location: Virtual
*Purpose: We describe the clinical presentation & immune response to COVID-19 infection in pediatric SOT.
*Methods: Medical records of COVID-19 PCR+ or seropositive patients were reviewed for details of their disease course. Blood was obtained during PCR or seropositivity for immunophenotyping & PlexCOVID-19 test. PlexCOVID-19 measures frequencies of spike Ag reactive T cells that express CD154. A pre-established algorithm predicts likelihood of COVID-19 severity. Controls were peds SOT patients with negative COVID-19 status. RNA isolated from liver tissue for PCR using the Lyra SARS CoV-2 Assay. As induction of immunological memory is central to anti-pathogen adaptive immunity induced by infection, IHC of liver tissue for tissue resident memory cells (TRM) (defined as CD69+ expressing CD4 or CD8 T cells) was performed.
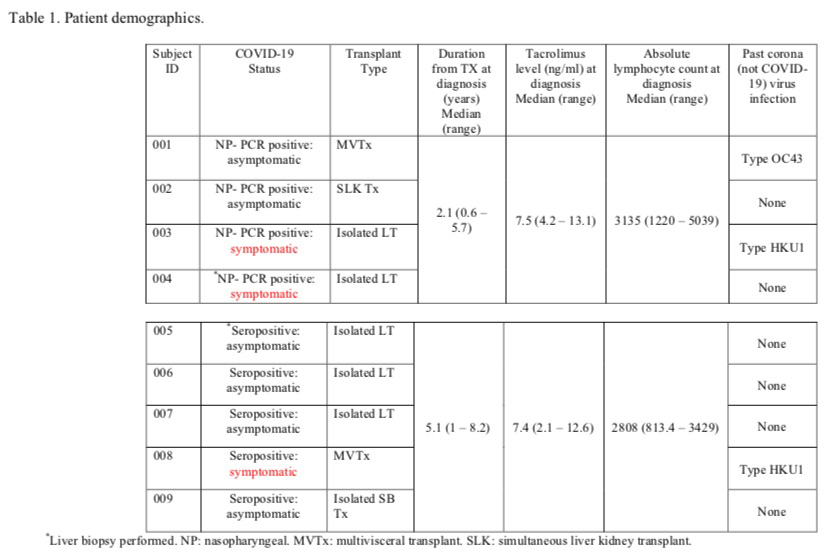
*Results: 4 patients had COVID-19 & 5 patients were seropositive between March & Nov 2020 (Table 1). The 2 symptomatic PCR+ patients were hospitalized for 24-48-hours & the symptomatic seropositive patient had a prolonged PICU stay. Steroid was discontinued in 1 symptomatic PCR+ patient; & target CNI goal & steroid dose decreased in the symptomatic seropositive patient due to concurrent BK viremia. 8 patients remain well at home. Histology on 1 symptomatic PCR+ patient with elevated LFT’s revealed lymphocytic portal inflammation & SARS CoV-2 PCR on the liver was negative; histology on 1 asymptomatic seropositive patient was normal. Infrequent TRM were seen on liver biopsies but were increased in PCR+ & seropositive biopsies vs. biopsies from same patients that pre-date a COVID-19+ status. CD4+ T cells in PCR+ & seropositive patients had a phenotype consistent with activation, including expression of HLA-DR (p = 0.008); Further, BST2 was constitutively expressed on a subset of CD4+ T cells in PCR+ patients reflecting a history of IFN-alpha induced signals (p=0.01). The frequencies of spike Ag-reactive CD3 (0.95 ± 0.35 vs 2.73 ± 0.35, p= 0.037) and CD8 cells (1.10 ± 0.70 vs 5.03 ± 0.80, p= 0.034) were lower in symptomatic PCR+ patients compared with asymptomatic seropositive subjects.
*Conclusions: A small number of our SOT patients had mild or asymptomatic COVID-19 infection, with notable activation of CD4+ T cells, & constitutive expression of BST2 reflecting IFN-alpha induced signals. Spike-antigen-reactive T-cells was lower during symptomatic vs. asymptomatic infection.
To cite this abstract in AMA style:
Ekong U, Paul S, Royal S, Chahine J, Yazigi N, Kaufman S, Khan K, Matsumoto C, Kroemer A, Fishbein T. Should We Worry About Covid-19 Infection in Pediatric SOT? [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/should-we-worry-about-covid-19-infection-in-pediatric-sot/. Accessed February 20, 2026.« Back to 2021 American Transplant Congress