Should We Curtail the Importance of Non-modifiable Risk Factors in Dcd Liver Risk Stratification?
1University of Maryland, Baltimore, Baltimore, MD, 2UCSF, San Francisco, CA
Meeting: 2021 American Transplant Congress
Abstract number: 477
Keywords: Bile duct, Donors, non-heart-beating, Liver, Outcome
Topic: Clinical Science » Liver » Liver: MELD, Allocation and Donor Issues (DCD/ECD)
Session Information
Session Time: 7:30pm-8:30pm
 Presentation Time: 8:00pm-8:10pm
Presentation Time: 8:00pm-8:10pm
Location: Virtual
*Purpose: Scoring systems have been proposed to select donation after circulatory death (DCD) donors and recipients for liver transplantation (LT). We hypothesized that the generalizability of existing scoring systems is limited by distinct local factors such that conforming to a complex scoring system derived elsewhere may limit transplantation.
*Methods: We used the University of California San Francisco (UCSF) data on DCD-LT (n=138) performed between 2003-2019 to calculate a UCSF-DCD risk score. This was validated using the United Network for Organ Sharing database (UNOS) (n=6,371). We compared the ability to predict graft survival of different scoring systems including United Kingdom (UK)-DCD-score, University of California Los Angeles (UCLA)-DCD-score, King’s College Hospital score (KCH)-DCD-score and UCSF-DCD-score in both datasets.
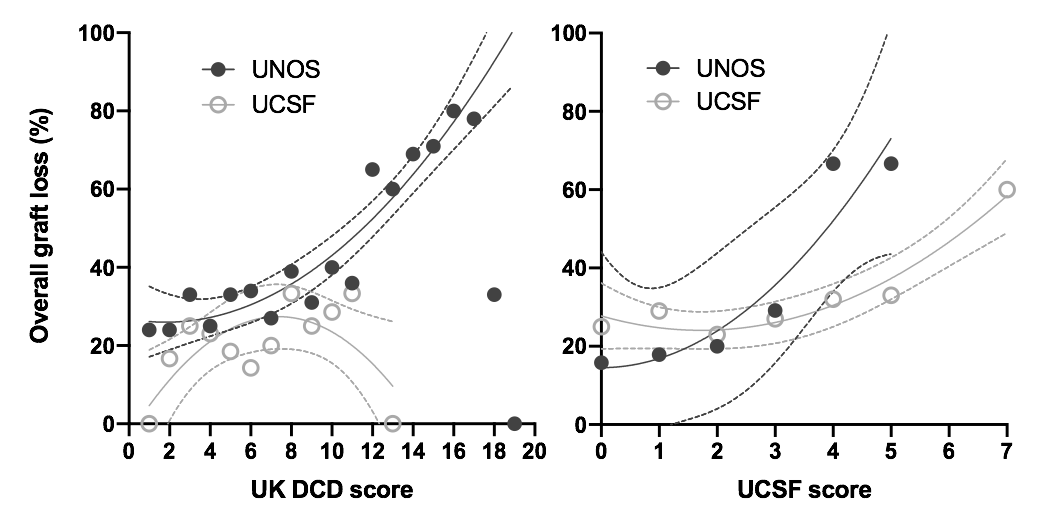
*Results: The strongest predictors in the UCSF cohort were donor functional warm ischemia time and donor hepatectomy time. A simple UCSF-DCD-score composed of just these two variables was able to stratify graft survival in our cohort and in the UNOS cohort (Figure). UK-, UCLA-, KCH-DCD-scores all successfully stratified graft survival in the UNOS cohort but failed to do so in the UCSF cohort. There was substantial variation in the ability of scoring systems to predict outcomes across UNOS regions. Based on the UK-DCD score, 43.5% of the DCD-LTs in the UCSF cohort were considered high-risk or futile. Specifically, 41.3% of recipients had a Model for End-Stage Liver Disease score>25 and 76.8% of LTs had cold ischemia time>6h; on the other hand, donor mean age was 31 years old, i.e. 18 years younger than the UK cohort average. UCSF-DCD-score was the only score able to stratify the occurrence of biliary complications in our cohort.
*Conclusions: Locally developed DCD scores failed to predict outcomes in our cohort, suggesting that extrapolation of locally derived DCD risk scores to other environments could limit transplantation. Additionally, the importance of non-modifiable factors should be minimized in DCD-scoring systems, and priority given to modifiable factors, such as donor warm ischemia and hepatectomy time.
To cite this abstract in AMA style:
Meier R, Kelly Y, Yamaguchi S, Braun H, Lunow-Luke T, Adelmann D, Niemann C, Maluf D, Dietch Z, Stock P, Kang S, Feng S, Posselt A, Gardner J, Freise C, Hirose R, Freise C, Ascher N, Roberts J, Roll G. Should We Curtail the Importance of Non-modifiable Risk Factors in Dcd Liver Risk Stratification? [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/should-we-curtail-the-importance-of-non-modifiable-risk-factors-in-dcd-liver-risk-stratification/. Accessed July 5, 2025.« Back to 2021 American Transplant Congress