Pro Inflammatory Transitional B (TrB) Cells Characterize Renal Allograft Recipients with DSA and T Cell Mediated Rejection (TCMR).
UPMC, Pittsburgh
Meeting: 2017 American Transplant Congress
Abstract number: D117
Keywords: Alloantibodies, B cells, FACS analysis, Rejection
Session Information
Session Name: Poster Session D: Kidney: Acute Cellular Rejection
Session Type: Poster Session
Date: Tuesday, May 2, 2017
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall D1
De novo DSA detected post-renal transplantation is associated with adverse outcomes. We have shown that de novo DSA is strongly associated with TCMR. In this prospective longitudinal study, we further studied the association between DSA, TCMR and renal function at 2yrs and examined their relationship to the peripheral blood B cell cytokine profile at 3mo (a measure of immunological reactivity).
Patients were screened for DSA with blood draws at 0,1,3,6,9,12 & 18mo. Rejection was diagnosed with 2 protocol biopsies (Bx) (3&12mo) and any for-cause Bx. IS was with Thymo and MPA+TAC. 79 (21%) of 372 patients transplanted between 1/13 & 12/14 developed de novo DSA. DSA was detected early (<3mo) in 62% (49/79) of these patients. Of those with DSA, 40 (51%) had acute rejection (88%TCMR, 12%TCMR+AMR) in the 1st year. In 86% (30/35) of these patients, DSA developed prior to or concomitant with TCMR diagnosis (DSA->TCMR). In contrast, in patients without DSA, 29% (86/293) had AR. Patients with DSA->TCMR had significantly worse serum creatinine and chronicity scores on 1yr biopsy than those with DSA or TCMR alone. Thus, DSA->TCMR identifies patients at higher risk of adverse outcomes and early diagnosis may allow timely intervention. Based on previous work, we analysed B cell subsets/cytokines at 3mo for their ability to risk stratify patients with DSA. Of the 34 patients with DSA who had PBMC available, 18 never had TCMR (DSA), and 16 had DSA->TCMR (4 had rejection at 3mo & 12 had subsequent rejection (6-12mo). Compared to patients with DSA alone, those with DSA->TCMR had significantly lower frequency of TrBs and these cells exhibited a more pro-inflammatory cytokine profile (reduced IL-10/TNFa ratio). Interestingly, in the small cohort of 12 patients with DSA->TCMR, the T1B cell IL-10/TNFa ratio was a good predictor for subsequent (6-12mo) TCMR (ROC AUC 0.82, p=0.01).
Conclusion: de no DSA->TCMR represents a high-risk population for adverse graft outcomes. These patients exhibit reduced TrB cells with a more pro-inflammatory cytokine profile. Analysis in more patients and time points will determine whether this marker can identify patients with DSA at risk for TCMR to prevent graft damage.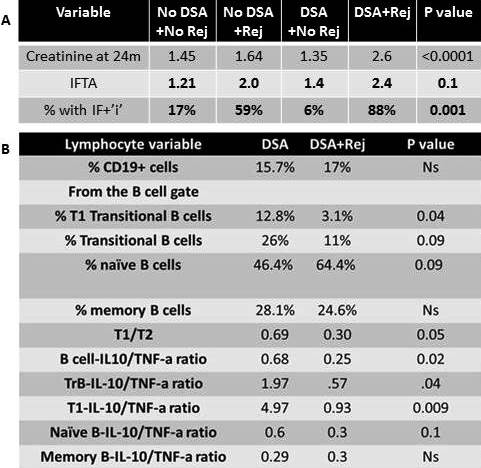
CITATION INFORMATION: Sharma A, Cherukuri A, Rothstein D. Pro Inflammatory Transitional B (TrB) Cells Characterize Renal Allograft Recipients with DSA and T Cell Mediated Rejection (TCMR). Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Sharma A, Cherukuri A, Rothstein D. Pro Inflammatory Transitional B (TrB) Cells Characterize Renal Allograft Recipients with DSA and T Cell Mediated Rejection (TCMR). [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/pro-inflammatory-transitional-b-trb-cells-characterize-renal-allograft-recipients-with-dsa-and-t-cell-mediated-rejection-tcmr/. Accessed July 15, 2025.« Back to 2017 American Transplant Congress
