Primary Graft Dysfunction in a Risk-Stratified vs. Routine Induction Protocol in Heart Transplant Recipients
1Baylor Scott & White Research Institute, Dallas, TX, 2Texas A&M University College of Medicine Health Science Center, Dallas, TX, 3Baylor Scott & White Health, Dallas, TX
Meeting: 2021 American Transplant Congress
Abstract number: 1194
Keywords: Graft function, Heart transplant patients, Induction therapy
Topic: Clinical Science » Heart » Heart and VADs: All Topics
Session Information
Session Name: Heart and VADs: All Topics
Session Type: Poster Abstract
Session Date & Time: None. Available on demand.
Location: Virtual
*Purpose: Treatment of left ventricular primary graft dysfunction (PGD-LV) is supportive in nature. We aim to evaluate whether a change in induction protocol from a routine to risk stratified (RSI) approach resulted in a change in prevalence of PGD-LV or inotrope score.
*Methods: We retrospectively reviewed consecutive first-time heart transplant recipients between January 2015 and February 2019. PGD-LV was graded according to the ISHLT-2014 criteria. Survival and biopsy-proven acute cellular (ACR≥2R) and antibody-mediated rejection (pAMR>0) were assessed to 1 year post-transplant. Baseline recipient and donor characteristics, and PGD-LV were compared between protocols using chi-square, Fisher Exact, Wilcoxon, and t-tests. Rank-based analysis of covariance was used to compare inotrope score adjusted for confounders. Time to event outcomes were analyzed using Cox proportional hazard models adjusted for moderate-severe PGD-LV.
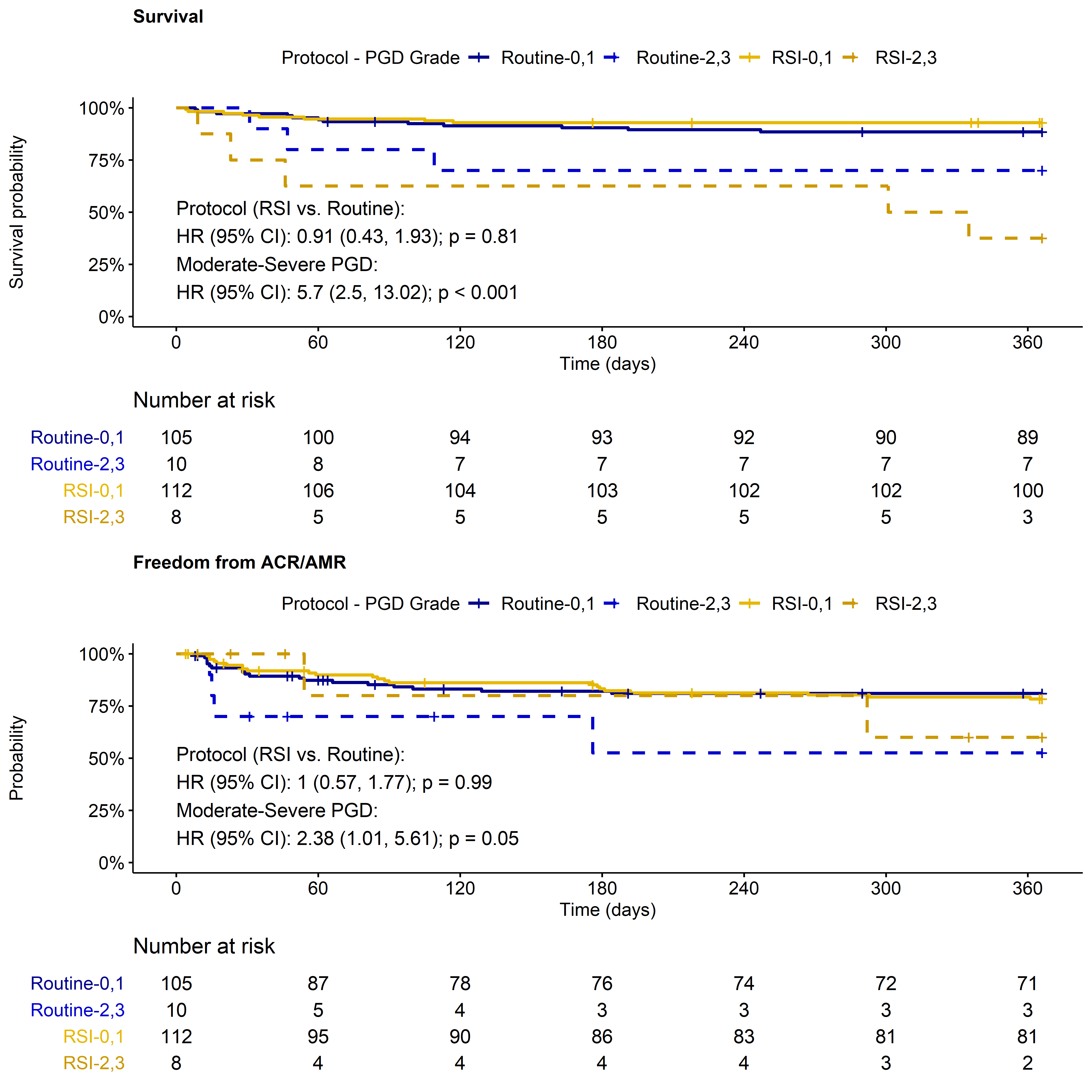
*Results: Of 235 recipients, 115 followed a routine induction protocol and 120 the RSI protocol implemented in 2017. In the routine group, 111 (97%) were treated with Basiliximab and 4 (3%) with Anti-thymocyte globulin (ATG); whereas 17 (14%) received Basiliximab, 2 (2%) ATG and 101 (84%) no induction therapy in the RSI group. Baseline recipient and donor characteristics were similar, except significantly higher mean arterial pressure (median [Q1-Q3]: 87 [81 – 97] vs. 83 [76 – 90] mmHg; p=0.01), fewer donors with left ventricular hypertrophy (LVH) (11% vs. 26%; p=0.008) and lower ischemic time (median [Q1 – Q3]: 179 [136, 225] vs. 209 [169, 247] min; p<0.001) in the RSI cohort. The prevalence of PGD-LV was similar (RSI vs. routine: 17% vs. 18%; p=0.88) and was composed of 23 mild, 6 moderate and 12 severe cases. In contrast, the median [Q1-Q3] inotrope score of 11 [7-14] in the RSI group was lower compared to 12 [9-17] in the routine group (p=0.02) which remained significant adjusting for donor LVH and ischemic time. The risk of mortality and of rejection between RSI and routine cohorts were similar when adjusting for moderate-severe PGD (p=0.81 and p=0.99; Fig.1).
*Conclusions: The RSI approach was associated with a reduction in induction therapy usage without an increase in PGD-LV. Risk of rejection and mortality adjusting for PGD-LV severity appears comparable between induction strategies. Moreover, a small reduction in the inotrope score was observed in the RSI cohort warranting further investigation.
To cite this abstract in AMA style:
Zyl JSvan, Zafar H, Nguyen PM, Felius J, Sam T, Hall SA. Primary Graft Dysfunction in a Risk-Stratified vs. Routine Induction Protocol in Heart Transplant Recipients [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/primary-graft-dysfunction-in-a-risk-stratified-vs-routine-induction-protocol-in-heart-transplant-recipients/. Accessed July 15, 2025.« Back to 2021 American Transplant Congress