Pre-transplant Prognostic Nutritional Index Predicts Short-term Outcomes After Liver Transplantation
E. Lisznyai, T. Kitajima, K. Delvecchio, A. Mohamed, S. Yeddula, T. Shamaa, T. Ivanics, K. Collins, M. Rizzari, A. Yoshida, M. Abouljoud, S. Nagai
Transplant Institute, Henry Ford Hospital, Detroit, MI
Meeting: 2021 American Transplant Congress
Abstract number: 1150
Keywords: Liver metabolism, Liver transplantation, Lymphocytes, Risk factors
Topic: Clinical Science » Liver » Liver: MELD, Allocation and Donor Issues (DCD/ECD)
Session Information
Session Name: Liver: MELD, Allocation and Donor Issues (DCD/ECD)
Session Type: Poster Abstract
Session Date & Time: None. Available on demand.
Location: Virtual
*Purpose: To understand the importance of pre-transplant nutritional status in optimizing liver transplant outcomes.
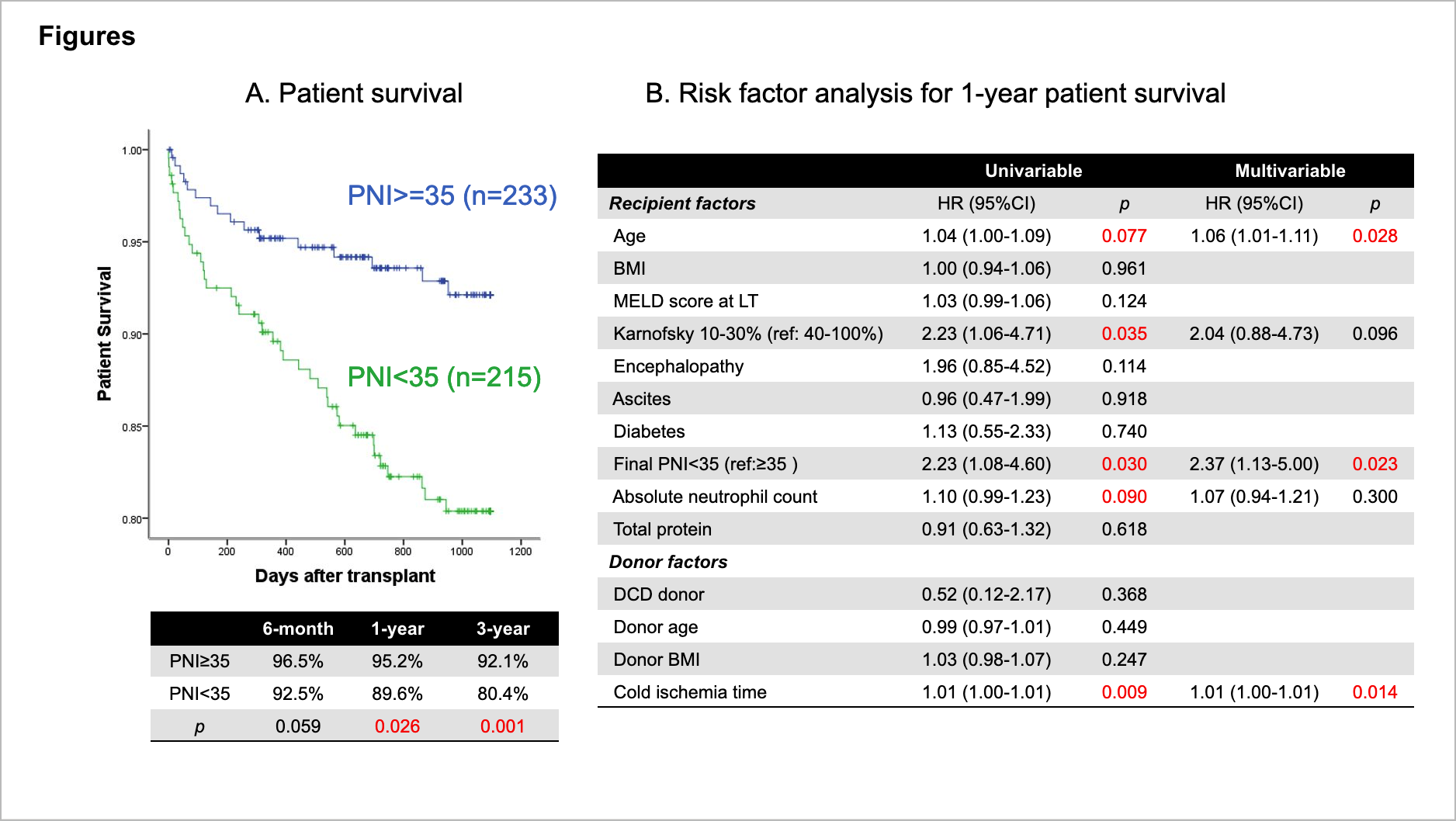
*Methods: The prognostic nutritional index (PNI) is a serum marker of nutrition and inflammation. We hypothesized pre-transplant PNI would predict short-term post-LT outcomes in deceased donor liver transplant (DDLT) patients. 451 patients underwent primary DDLT between 2013-2018 at our center. Re-transplants, multi-organ transplants and living donor liver transplants were excluded. Pre-transplant PNI = (10)*[albumin (g/dL)] + (0.005)*[Total Lymphocyte Count (/µL)]. PNI was analyzed as both a continuous and categorical variable. ROC curves yielded an optimal PNI cutoff of 35 to compare short-term outcomes between PNI≥35 and PNI<35 cohorts. Risk factors for patient death within 1-year were analyzed using Cox regression models and adjusted by recipient factors at LT.
*Results: Multivariable analysis associated PNI with 1-year survival as a continuous variable (HR=0.94, 95% CI=0.90-0.98; p=0.007). Of 451 patients, 215 (47.7%) had PNI<35. MELD score at time of transplant was higher in PNI<35 (22 vs. 19; p=0.028). Recipient age, gender, BMI, donor age, rates of diabetes mellitus and donors after cardiac death were equivocal. PNI<35 demonstrated lower 1-year survival (89.6% vs. 95.2%; p=0.026, Figure A). After risk adjustment, PNI<35 showed higher risk of 6-month (HR=2.44; p=0.047) and 1-year death (HR=2.47; p=0.018). Multivariable analysis revealed PNI<35 at LT (HR=2.37; p=0.023) was an independent risk factor for patient death within 1 year (Figure B).
*Conclusions: Lower pre-transplant PNI portended worse short-term survival in DDLT patients. PNI may be useful in evaluating pre-transplant nutritional status and optimizing LT outcomes.
To cite this abstract in AMA style:
Lisznyai E, Kitajima T, Delvecchio K, Mohamed A, Yeddula S, Shamaa T, Ivanics T, Collins K, Rizzari M, Yoshida A, Abouljoud M, Nagai S. Pre-transplant Prognostic Nutritional Index Predicts Short-term Outcomes After Liver Transplantation [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/pre-transplant-prognostic%e2%80%af-nutritional%e2%80%af-index%e2%80%af-predicts-%e2%80%afshort-term%e2%80%af-outcomes%e2%80%af-after-%e2%80%afliver-transplantation/. Accessed March 4, 2026.« Back to 2021 American Transplant Congress