Portal Vein Thrombosis and DCD Liver Transplantation: Dangerous Combination or Clinical Opportunity?
1General Surgery, Mayo Clinic, Phoenix, AZ, 2Mayo Clinic, Phoenix, AZ, 3Urology, Mayo Clinic, Phoenix, AZ, 4Mayo Clinic Alix School of Medicine, Phoenix, AZ
Meeting: 2022 American Transplant Congress
Abstract number: 421
Keywords: Graft survival, Liver, Liver transplantation, Outcome
Topic: Clinical Science » Liver » 55 - Liver: Recipient Selection
Session Information
Session Name: Recipient Selection
Session Type: Rapid Fire Oral Abstract
Date: Tuesday, June 7, 2022
Session Time: 3:30pm-5:00pm
 Presentation Time: 4:00pm-4:10pm
Presentation Time: 4:00pm-4:10pm
Location: Hynes Room 312
*Purpose: Individually, recipient portal vein thrombosis (PVT) and donation after circulatory death (DCD) allografts are associated with a higher risk of poor deceased donor liver transplant (DDLT) outcomes, leading to both waitlist mortality and organ discard. There are limited data on utilization and outcomes of DCD liver transplantation in the setting of PVT.
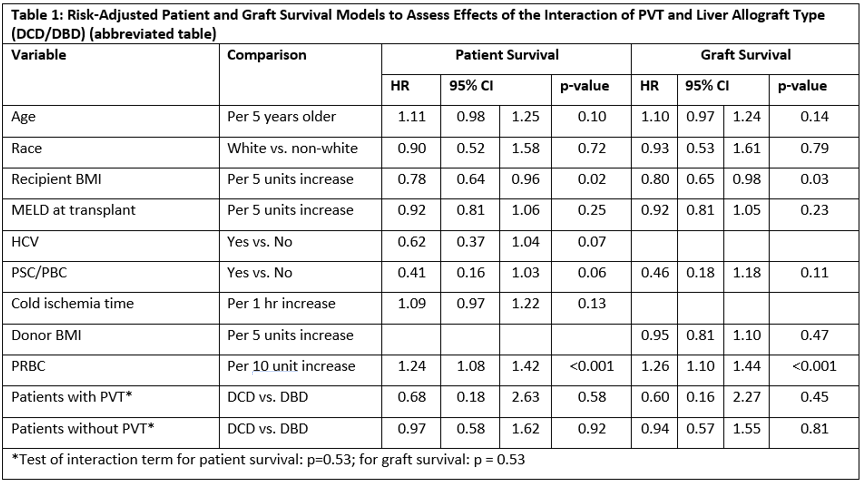
*Methods: We performed a retrospective, single-center cohort study of primary DDLTs (2014-2020) using granular clinical data and UNOS registry on recipients and donors. The primary variables of interest were PVT (classified by the Yerdel model) and allograft type (DCD or DBD). Using univariate and multivariate statistics, we measured differences in perioperative and post-operative outcomes stratified by the exposure variables. We developed risk-adjusted time-to-event models for graft and patient survival to assess the effect of PVT on outcomes in the setting of DBD or DCD liver allografts.
*Results: A total of 870 DDLT patients were identified. 16.4% (n=143) had PVT (Type I 62%, Type II 27%, Type III 10%, Type IV 1%). DCD LT was frequent overall (n=291, 33.7% of DDLT), 18% of DCD LT was for PVT patients (DCD-PVT n= 53). PVT status was not associated with differences in recipient age, sex, BMI, median MELD at transplant (19, IQR 13-25), vascular or biliary reconstruction approaches, median CIT (5.8 hrs, IQR 4.9-7.3)(all, p>0.05). PVT patients had significantly intraoperative higher blood product transfusion vs non-PVT patients (cryoprecipitate (p=< 0.001), FFP (p=0.003), PRBC (p=0.022)). 11.1% (n=16) PVT patients required radiological portal vein intervention within 4 months of DDLT (2.9% non-PVT, p<0.001), and was proportionally higher in Type II PVT (13.9%, n=5) vs other PVT groups. Of PVT patients requiring post-DDLT PV intervention, 21% were in DCD LT. After risk-adjustment with interaction terms (Table 1), PVT-DCD was not associated with an increased risk of post-DDLT mortality (HR 0.68 95% CI 0.18-2.63) or graft loss (HR 0.60, 95% CI 0.16-2.27), but higher recipient BMI and PRBC transfusion were associated with poorer outcomes. In non-PVT patients, DCD LT had similar risk-adjusted graft and patient survival vs. DBD-LT patients.
*Conclusions: In selected PVT patients in a high volume DDLT center, DCD LT had similar patient and graft survival outcomes as DBD LT. DCD liver allografts should be considered a viable donor source for these patients.
To cite this abstract in AMA style:
Calderon E, Chang Y, Lu P, Durant AM, Derakshani D, Anderson ML, Villa ERLuque, Jadlowiec C, Reddy K, Moss A, Mathur AK. Portal Vein Thrombosis and DCD Liver Transplantation: Dangerous Combination or Clinical Opportunity? [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/portal-vein-thrombosis-and-dcd-liver-transplantation-dangerous-combination-or-clinical-opportunity/. Accessed March 5, 2026.« Back to 2022 American Transplant Congress