Paired Surveillance Biopsies Over >4 Years from a Multi-Center Cohort of 78 Long-Term Pediatric Liver Transplant Recipients
1UCSF, San Francisco, CA, 2King's College, London, United Kingdom, 3Mt. Sinai School of Medicine, NY, NY, 4U of Pittsburgh, Pittsburgh, PA, 5Columbia U, NY, NY, 6Northwestern U, Chicago, IL
Meeting: 2021 American Transplant Congress
Abstract number: 1174
Keywords: Fibrosis, Graft survival, Liver transplantation, Pediatric
Topic: Clinical Science » Liver » Liver: Pediatrics
Session Information
Session Name: Liver: Pediatrics
Session Type: Poster Abstract
Session Date & Time: None. Available on demand.
Location: Virtual
*Purpose: Progressive liver fibrosis threatens graft and patient longevity for children after liver transplantation (LT). Previous studies are limited to single-center, cross-sectional analyses. To address this knowledge gap, we examined prevalence of progressive allograft fibrosis in sequential surveillance biopsies from 78 pediatric LT recipients from 11 centers.
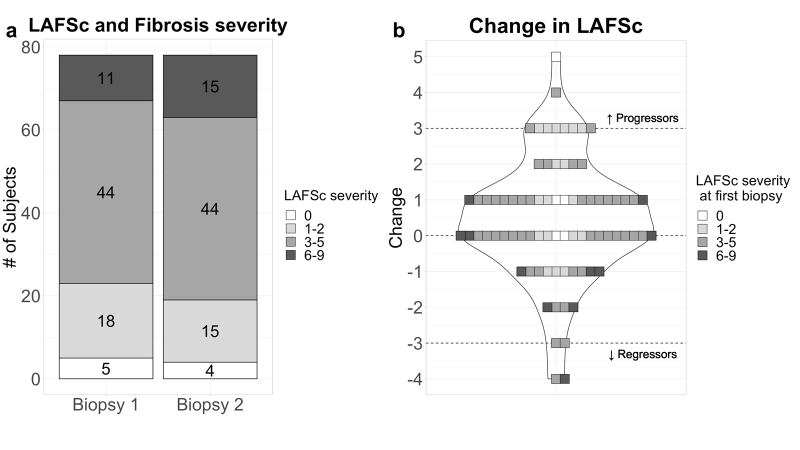
*Methods: Biopsies from 78 children (43 prospectively, 35 retrospectively, 0 LT for viral or autoimmune hepatitis) assessed by 1 central pathologist; paired biopsies compared side-by-side. Serum ALT and GGT levels were <40 U/L, index biopsy ≥4 yrs after LT, 2nd biopsy ≥4 yrs later. Fibrosis was staged by the liver allograft fibrosis score (LAFSc 0-9; 0 none, mild 1-2, moderate 3-5; severe 6-9) on H&E, trichrome stains. Significant fibrosis progression or regression was defined as LAFSc increase or decrease by ≥3.
*Results: Of 78 children, 51 were male, 44 had biliary atresia, 50 had living donors. Index biopsy was done at a median (IQR) 8.2 (5.9-11.6) yrs after LT with 89% on immunosuppression monotherapy, ALT 24 (19-35), GGT 15 (12-22) U/L. Fibrosis was none/mild in 29%, moderate in 56%, and severe in 14%. 2nd biopsy was done a median (IQR) of 4.7 (4.3-5.1) yrs later, at 13.8 (10.9-16.8) after LT, with 91% on monotherapy, ALT 25 (19-37), and GGT 17 (14-28) U/L. The majority (56%) had minimal LAFSc change (-1, 0, +1; FIGURE): 10 (13%) progressed (7 mild to mod) and 4 (5%) regressed (mod to mild). After adjusting for baseline LAFSc, progression was associated with younger age at LT [median (IQR) 0.7 (0.6-1.0) vs. 1.3 (0.6-2.0) yrs; p=0.02] but not with donor/graft type, time from LT to 1st or 2nd biopsy, time between biopsies, or ALT/GGT/inflammation at 1st biopsy. None had biliary or vascular complications. 8 of 10 with progression were on less IS at 2nd biopsy, as were 33% of those with stable/improved fibrosis.
*Conclusions: In our multicenter cohort, at 8 and 14 years after LT, only 14% and 19% respectively, of surveillance biopsies showed severe fibrosis. Progression was uncommon, seen in only 13%. This differs distinctly from previously reported cohorts, which may reflect a more modern, tacrolimus-based regimen and the subset of children studied. Our low prevalence of severe or progressive fibrosis suggests that non-invasive fibrosis assessment could be a useful adjunct in long-term monitoring for children with normal transaminases.
To cite this abstract in AMA style:
Perito ER, Persyn E, Bucuvalas J, Squires JE, Martinez M, Mohammad S, Demetris AJ, Feng S. Paired Surveillance Biopsies Over >4 Years from a Multi-Center Cohort of 78 Long-Term Pediatric Liver Transplant Recipients [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/paired-surveillance-biopsies-over-4-years-from-a-multi-center-cohort-of-78-long-term-pediatric-liver-transplant-recipients/. Accessed February 19, 2026.« Back to 2021 American Transplant Congress