Outcomes of Small-for-Size Grafts in Adult Living Donor Liver Transplantation.
1Columbia University Medical Center, New York
2Weill Cornell Medical College, New York.
Meeting: 2016 American Transplant Congress
Abstract number: A210
Keywords: Donation, Graft survival, Liver, Weight
Session Information
Session Name: Poster Session A: Living Donor Liver Transplantation
Session Type: Poster Session
Date: Saturday, June 11, 2016
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Halls C&D
Lower limit of graft size in adult Living donor liver transplantation (LDLT) is not well established. This study examines the outcomes with use of small-for-size grafts (SFSGs) in LDLT in a single center. Graft-to-recipient weight ratio (GRWR) of less than 0.8 was designated as SFSG. From 2002-15, 41 cases of adult-to-adult LDLT with a GRWR of <0.8 were performed at the center. These constituted 24 left lobes. These were compared to all adult LDLTs with GRWR >/=0.8 (n=95) carried out in the same time period. Median follow-up duration was 3.1 years. Mean GRWR of SFSGs was 0.66 versus 1.06 (p<0.0001) in the larger graft group. SFSGs consisted of significantly more left lobes (58.5% versus 21%, p<0.0001) as compared to the larger group. HCV and HCC constituted a significantly higher proportion of cases in the smaller group (60.9% versus 42.1%, p=0.043, 34% versus 16.8%, p=0.026). Preoperative MELD scores were not different between the groups
| Characteristic | GRWR <0.8 (mean) n=41 | GRWR >/=0.8 (mean) n=95 | p value |
| Age (yrs) | 52.5 | 52.56 | 0.99 |
| Mean graft weight (gms) | 525 | 781.38 | <0.0001 |
| Mean GRWR | 0.667 | 1.06 | <0.0001 |
| MELD | 15.6 | 15.6 | 0.979 |
| Small for size syndrome | 7.3% | 3.16% | 0.278 |
. Rate of biliary strictures was not different between the groups (39% versus 31.6%, p=0.4). Liver synthetic function and kidney function at 1 and 3-years post transplant were comparable between the groups. The 1 and 3-year graft survival for GRWR<0.8 group were 87% and 80% compared to 90% and 86% for the larger group (p=0.55) 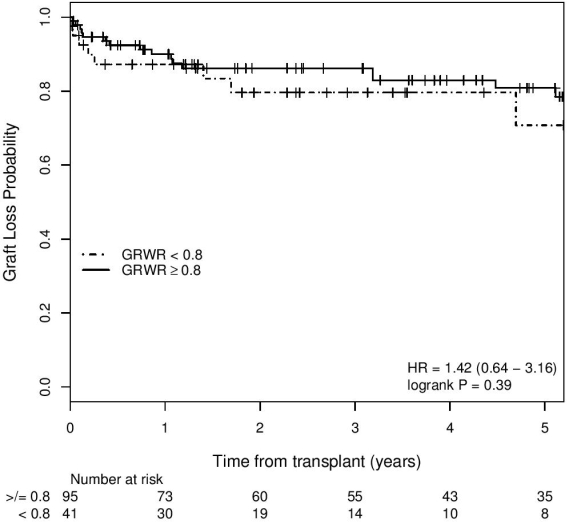 . The 1 and 3-year patient survival for GRWR<0.8 group were 89% and 82% compared to 92% and 88% for the larger group (p=0.55)
. The 1 and 3-year patient survival for GRWR<0.8 group were 89% and 82% compared to 92% and 88% for the larger group (p=0.55) 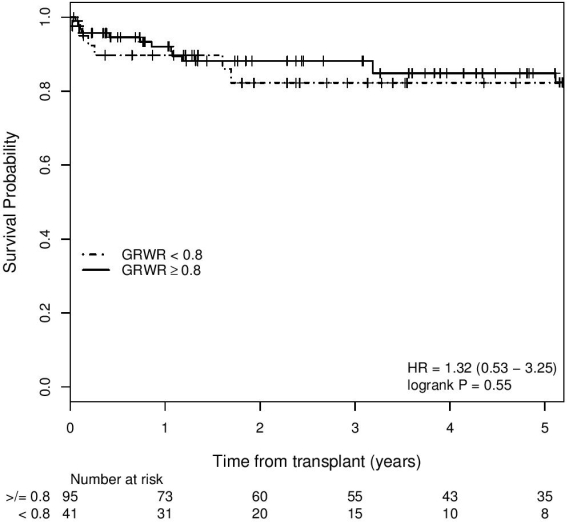 . Use of smaller grafts composed predominantly of left lobes had comparable outcomes with larger grafts and potentially expands applicability of LDLT.
. Use of smaller grafts composed predominantly of left lobes had comparable outcomes with larger grafts and potentially expands applicability of LDLT.
.
CITATION INFORMATION: Klair T, Przybyszewski E, Samstein B. Outcomes of Small-for-Size Grafts in Adult Living Donor Liver Transplantation. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Klair T, Przybyszewski E, Samstein B. Outcomes of Small-for-Size Grafts in Adult Living Donor Liver Transplantation. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/outcomes-of-small-for-size-grafts-in-adult-living-donor-liver-transplantation/. Accessed July 6, 2025.« Back to 2016 American Transplant Congress
