Nodular Regenerative Hyperplasia after Liver Transplant – It is All in the Presentation
1University of California, San Francisco - Fresno, Fresno, CA, 2University of California, San Francisco, San Francisco, CA
Meeting: 2019 American Transplant Congress
Abstract number: B311
Keywords: Graft failure, Graft survival, Liver transplantation
Session Information
Session Name: Poster Session B: Liver Retransplantation and Other Complications
Session Type: Poster Session
Date: Sunday, June 2, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall C & D
*Purpose: There is a paucity of data on nodular regenerative hyperplasia (NRH) after liver transplant (LT). We report the largest existing case series with extensive follow up to more clearly define the clinical presentations and outcomes of NRH that developed after LT.
*Methods: We retrospectively collected pre-, peri- and post-operative data from a single center between 1988 and 2018, concentrating on published postulated risk factors, time from LT to diagnosis, symptom complex and MELD-Na at the time of NRH diagnosis, need for re-LT, and patient and graft survival in adult recipients. Diagnosis of NRH was based on pathologic findings. Patients were divided into 1) early vs. late presentation (<48 months versus >48 months), and 2) asymptomatic (abnormal liver tests only) vs symptomatic (portal hypertension). Immune suppression was generally not adjusted after the diagnosis of NRH.
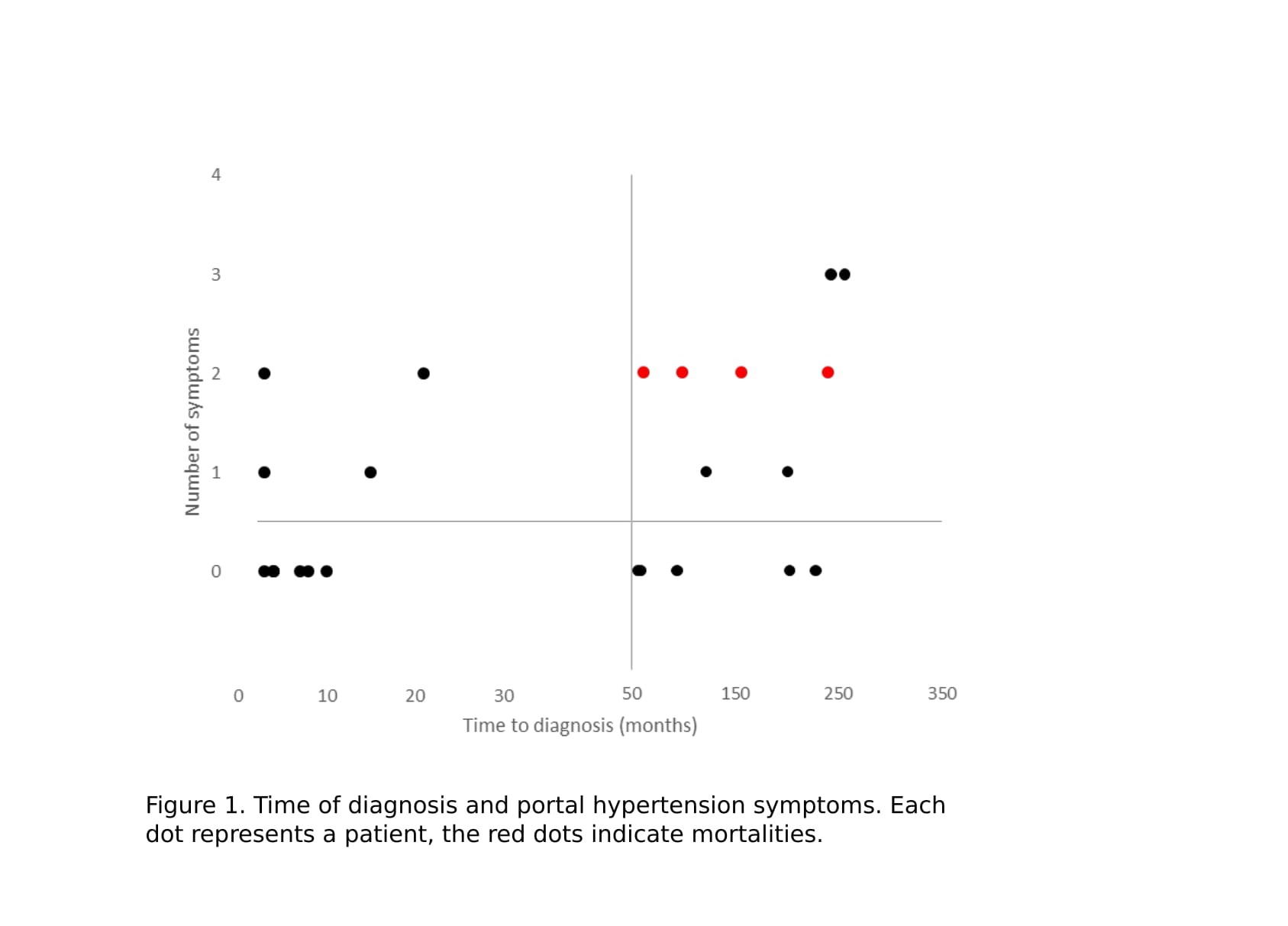
*Results: 24 patients with NRH after LT were identified (7 early asymptomatic, 4 early symptomatic, 4 late asymptomatic, and 9 late symptomatic). The mean age was 43 years at age of transplant, 11 (46%) were female. 19 patients received LT from deceased donors and 5 from living donors. The mean time of diagnosis of NRH after LT was 87 months (3-256 months). Our mean follow up time from time of transplant was 35.8 months (6-99 months). 7 patients (29%) (figure 1) had severe enough NRH to result in death (n=4, 17%) or were evaluated for re-LT (n=5, 21%). All 4 patients that died had a late symptomatic presentation (mean time to diagnosis in these 4 patients was 140 months). One patient received re-LT for NRH. MELD-Na scores at time of diagnosis (p=0.03), and 6-12 months after diagnosis (p=0.024) was significantly higher in the late symptomatic group. Of the existing postulated risk factors for NRH, 6 (25%) of our patients had some autoimmune disease, 4 (17%) were exposed to azathioprine, 2 (8%) had chemotherapy, 9 (38%) had been treated for rejection, and 7 (29%) patients had a vascular complication which required treatment. 4 (17%) patients had none of these risk factors. Rejection was significantly more common in the 7 patients who either died or were evaluated for re-LT (p=0.03). A notable patient had NRH twice.
*Conclusions: The etiology of NRH after LT remains poorly understood, but our results suggest a link to an immune-mediated process rather than vascular complication. Late symptomatic presentation was associated with poor prognosis.
To cite this abstract in AMA style:
Chen AK, Yamaguchi S, Praglin C, Agudelo E, Yao FK, Syed SM, Roll GR. Nodular Regenerative Hyperplasia after Liver Transplant – It is All in the Presentation [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/nodular-regenerative-hyperplasia-after-liver-transplant-it-is-all-in-the-presentation/. Accessed February 22, 2026.« Back to 2019 American Transplant Congress