Management of Orphan Ducts After Pediatric Living Donor Liver Transplantation
1Thomas E. Starzl Transplantation Institute, University of Pittsburgh Medical Center, Pittsburgh, PA, 2Hillman Center for Pediatric Transplantation, Children's Hospital of Pittsburgh of UPMC, Pittsburgh, PA, 3Department of Radiology, Children's Hospital of Pittsburgh of UPMC, Pittsburgh, PA
Meeting: 2019 American Transplant Congress
Abstract number: B351
Keywords: Bile duct, Liver transplantation, Pediatric
Session Information
Session Name: Poster Session B: Liver: Living Donors and Partial Grafts
Session Type: Poster Session
Date: Sunday, June 2, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall C & D
*Purpose: Living donor (LDLT) and split (SLT) livers are two technical variants of standard liver transplants that potentially increase the number of liver allografts available to children for transplantation. Multicenter studies suggest that technical variant grafts are associated with decreased graft survival and higher biliary complications. An excluded bile duct or “orphan duct” (OD) is a unique potential biliary complication in segmental transplantation.
*Methods: All pediatric end stage liver disease patients receiving LDLT were analyzed retrospectively for ODs. ODs are managed with a combined surgical and percutaneous transhepatic cholangiogram and percutaneous biliary drainage (PTC/PBD).
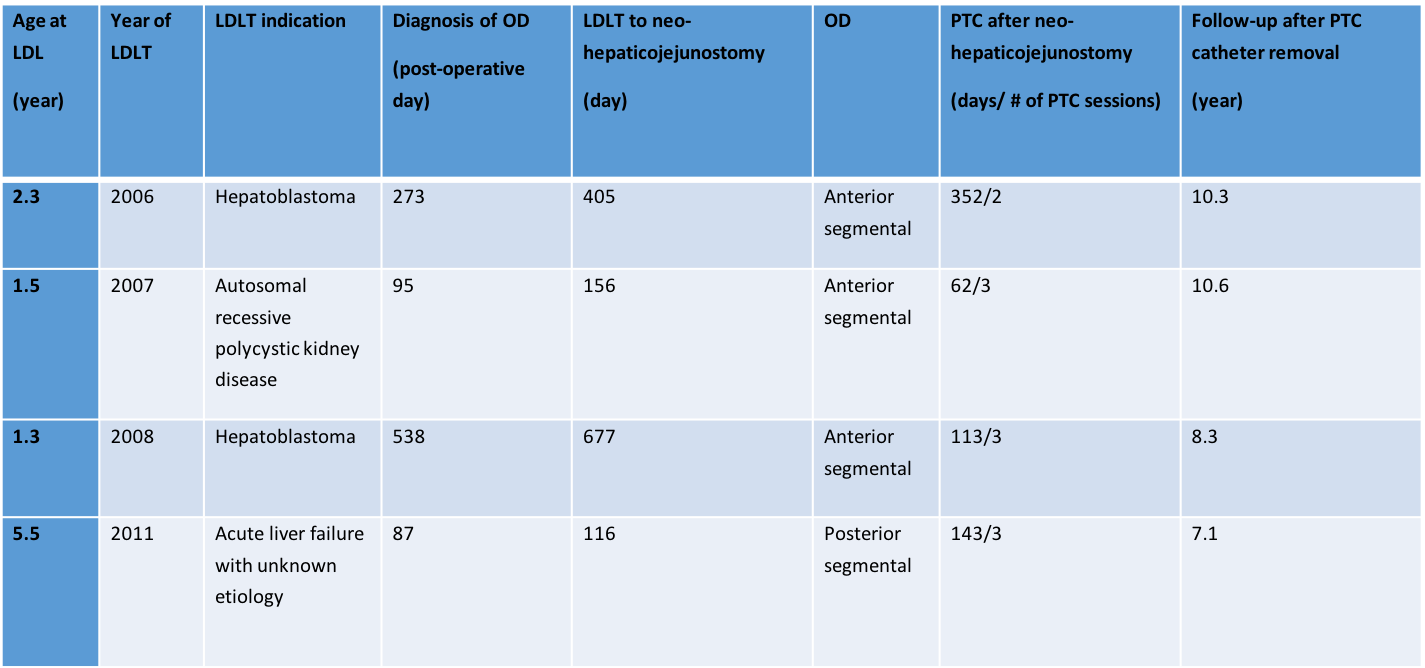
*Results: Between 1997 and November 2018, 127 children underwent living donor liver transplantation. Four patients were identified with excluded bile duct at time of left lateral segment LDLT. All ODs were evaluated with ultrasound, magnetic resonance cholangio-pancreatography (MRCP) and confirmed with percutaneous cholangiography. All patients managed by PTC/PBD at diagnosis then underwent operative exploration. A combined team of interventional radiology and transplant surgical staff was needed for restoration of biliary-enteric continuity via creation of a “neo-hepaticojejunostomy”. PBD was continued post-operatively and patients underwent serial dilatations. All patients are alive with good functioning grafts with normal liver function tests after prolonged follow-up. Liver biopsies have demonstrated only mild biliary ductular reaction without evidence of recurrence or significant biliary fibrosis. Pertinent data is summarized in the table.
*Conclusions: Orphan duct is a rare complication seen in pediatric liver transplantation. An awareness of this potential complication should promote early recognition and treatment. OD has been successfully managed with a combined surgical and interventional approach without significant graft dysfunction or graft loss.
To cite this abstract in AMA style:
Celik N, Ganoza A, Khanna A, Bond G, Soltys K, Sindhi R, Crowley J, Humar A, Mazariegos G. Management of Orphan Ducts After Pediatric Living Donor Liver Transplantation [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/management-of-orphan-ducts-after-pediatric-living-donor-liver-transplantation/. Accessed April 17, 2024.« Back to 2019 American Transplant Congress