Lung Mucosal Biopsies Deteriorate with Time Post-Transplant: A Molecular Analysis
1Alberta Transplant Applied Genomics Centre, Edmonton, AB, Canada, 2University of Alberta, Edmonton, AB, Canada, 3., ., AB, Canada
Meeting: 2020 American Transplant Congress
Abstract number: B-290
Keywords: Gene expression, Graft function, Lung transplantation, N/A
Session Information
Session Name: Poster Session B: Lung: All Topics
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Mucosal biopsies from the third airway bifurcation (3BMBs) assessed molecularly can be used to detect rejection (DOI: 10.1111/ajt.15685), and may also provide insights into injury. In the present study, we examined changes in injury-related transcripts in mucosal biopsies to see how the airways changed with time.
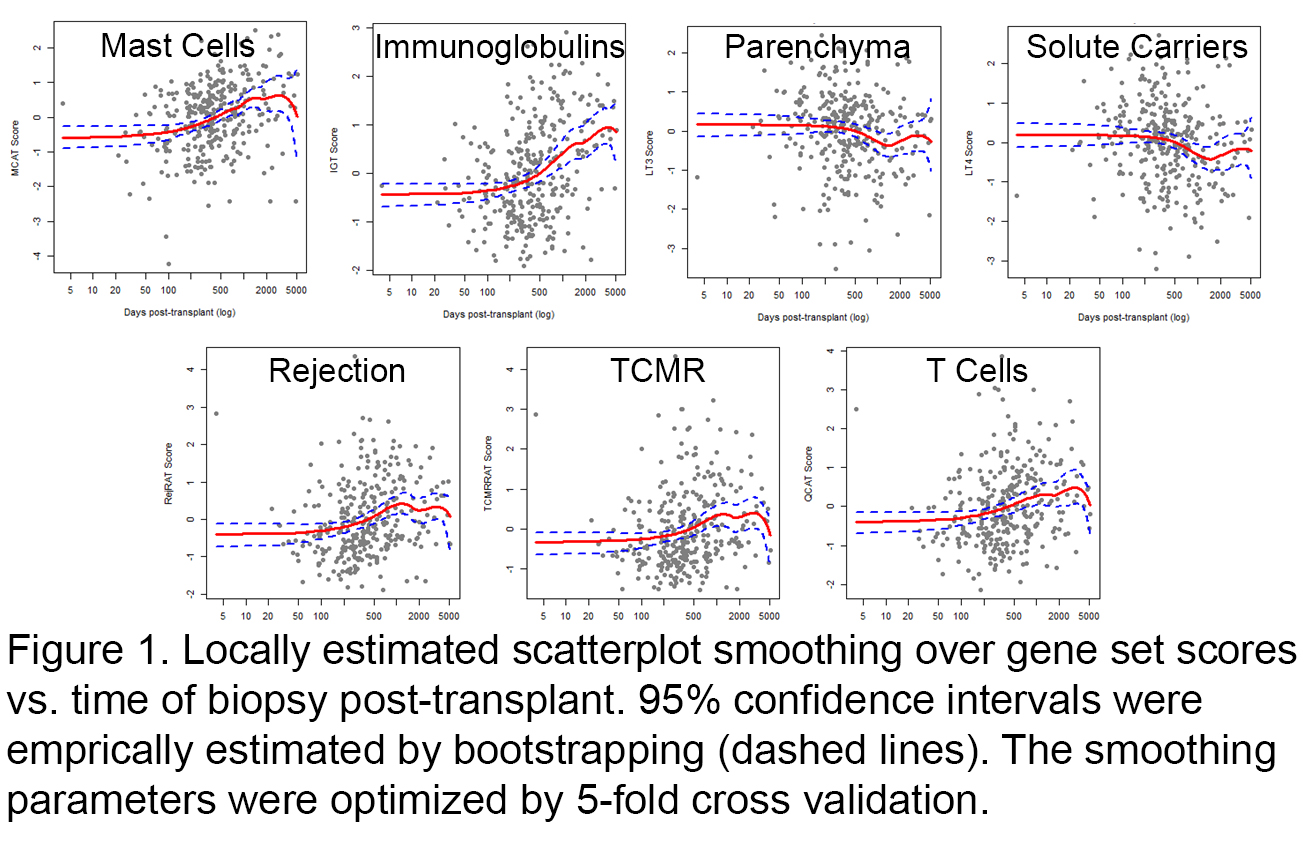
*Methods: We processed 314 3BMBs collected from 8 centers on gene expression microarrays. We studied the relationship of time of biopsy post-transplant to pathogenesis-based transcript set (PBT) scores representing injury and rejection. Linear 2-knot spline regression and locally estimated scatterplot smoothing (loess) were used to model the relationships and bootstrapped 95% confidence intervals (CI) estimated their robustness.
*Results: There was no discernible relationship between time post-transplant and scores in the first 210 days. Thereafter immunoglobulin and mast cell transcript scores trended upwards with good support from their loess CIs and statistically significant coefficients in linear spline regression (p<0.05). Rejection- and T cell-associated scores trended slightly upwards with and lung parenchymal transcripts downwards, signaling deterioration (epithelial de-differentiation). CLAD was correlated with time post-transplant (0.5), but not with a specific molecular phenotype (few biopsies with CLAD were available).
*Conclusions: Late mucosal biopsies demonstrated time-dependent molecular changes reminiscent of those observed in heart and kidney transplants with late atrophy/fibrosis: accumulation of immunoglobulins and T cells and parenchymal deterioration. Time accounted for a small amount of the total variance in gene expression, indicating that other factors contribute to the variation. These findings suggest that, in addition to rejection changes, specific patterns of gene expression – loss of parenchymal transcripts and increased immunoglobulin, mast cell, and T cell transcripts – can be monitored in the mucosa post-transplant to better understand the state of the airways.
To cite this abstract in AMA style:
Parkes MD, Halloran P, Halloran K. Lung Mucosal Biopsies Deteriorate with Time Post-Transplant: A Molecular Analysis [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/lung-mucosal-biopsies-deteriorate-with-time-post-transplant-a-molecular-analysis/. Accessed February 22, 2026.« Back to 2020 American Transplant Congress