Living Donor Renal Transplantation without Any Induction Immunosuppression in Spousal Donors – Single Center Experience
R. Bhat, F. Aziz, I. N. Abubecker, S. Narayanan, B. Hafeeque
Nephrology & Transplantation, Malabar Instiute of Medical Sciences, Calicut, India
Meeting: 2019 American Transplant Congress
Abstract number: B195
Keywords: Donors, unrelated, Graft survival, HLA antibodies, Induction therapy
Session Information
Session Name: Poster Session B: Kidney Immunosuppression: Induction Therapy
Session Type: Poster Session
Date: Sunday, June 2, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall C & D
*Purpose: Renal transplantation in India is primarily driven by living related donation; parents and spouse constitute 70% of donors in India. Some centres use induction immunosuppression (IIS) for all spousal transplants considering it as an immunologically high risk scenario. Our protocol is to give induction only if recipients are of immunologically high risk from anti-HLA antibody perspective. Objective: To compare the outcomes like incidence of rejection in the first post-transplant year, graft loss & patient loss among patients who have undergone renal transplantation from parental-donor and spousal-donor without any IIS.
*Methods: It is a retrospective study of living donor renal transplantation of parents & spouse (wife) as donors. Patients from Jan 2006 to Dec 2016 were included. We excluded patients with induction therapy, ABOi transplantation and female recipients with husband-donors who had pregnancy as sensitizing event.
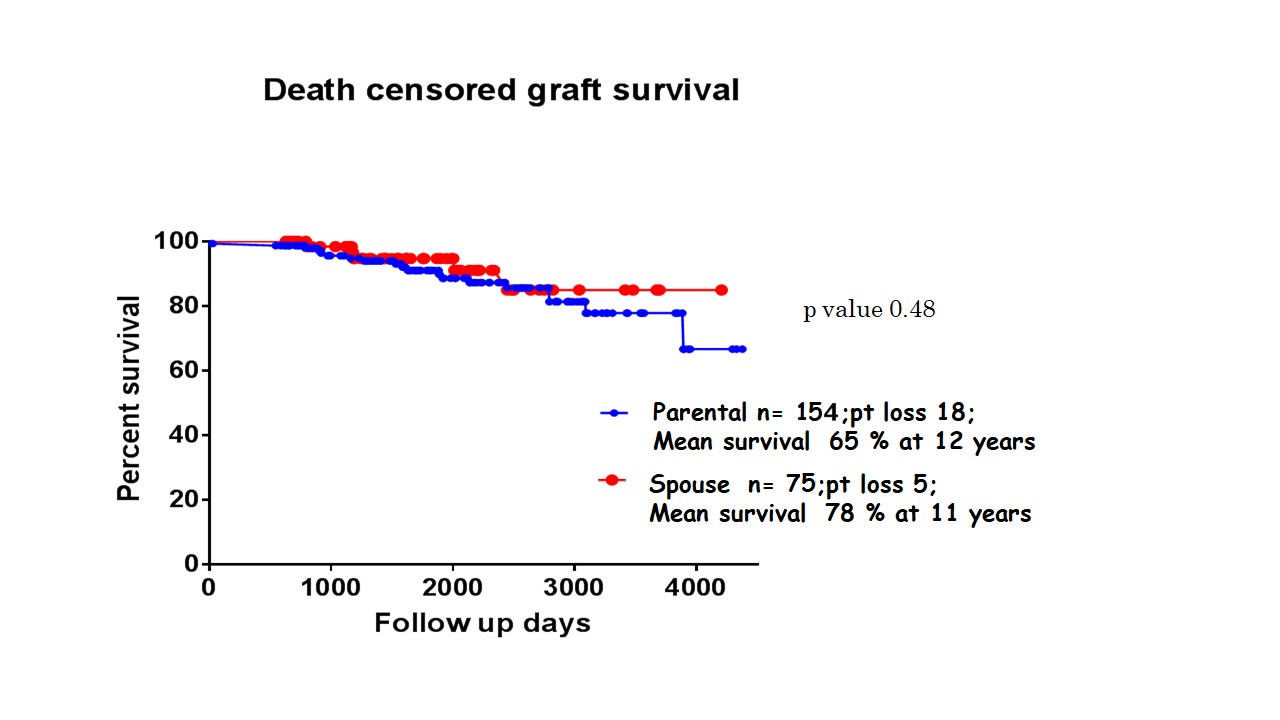
*Results: Out of 361 patients, 154 belonged to parental-donor and 75 patients to spousal-donor groups with average follow-up of 2009 ± 998 and 1740 ± 922 days respectively. The mean age of recipients was significantly lower in parent group (27.79 ±6.85 yrs) than in Spousal group (45.62±7.96yrs).Donor age was much higher in parent group (50.42 ± 7.32) than the spousal group (38.36±7.81). Spousal group received kidney with mean GFR was 48.98±43.27 which was significantly higher than the parent donor group 38.85 ± 9.26 (p=0.02). The incidence of acute rejections in the first post-transplant year were comparable with 18% in parent-donor and 17% in spousal-donor groups respectively. Of the rejections parental-donor had more cellular rejections; ABMR and mixed rejections were more common in spousal-donors. Patient-loss and “Death Censored Graft Loss” were comparable in both parent-donor and spouse-donor groups. 5 year patient survival was 95% and 92%; 5 year death censored graft survival was 87% and 91% in parental-donor and spousal donor groups respectively.
*Conclusions: The incidence of acute rejection, long term graft and patient survival of “immunologically low risk” recipients with spousal-donation without any induction IS were comparable to traditionally considered low-immunological risk parental-donation transplants. Spousal donation can provide more age compatible transplantations with better GFR compared to parental donation without augmented immunosuppression in patients with low immunological risk.
To cite this abstract in AMA style:
Bhat R, Aziz F, Abubecker IN, Narayanan S, Hafeeque B. Living Donor Renal Transplantation without Any Induction Immunosuppression in Spousal Donors – Single Center Experience [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/living-donor-renal-transplantation-without-any-induction-immunosuppression-in-spousal-donors-single-center-experience/. Accessed March 6, 2026.« Back to 2019 American Transplant Congress