Liver Transplantation for Primary Liver Sarcoma in Children-The US Experience from the Scientific Registry for Transplant Recipients (1988-2018)
University of Pittsburgh Medical Center, Pittsburgh, PA
Meeting: 2020 American Transplant Congress
Abstract number: B-144
Keywords: Liver, Liver transplantation, Malignancy, Pediatric
Session Information
Session Name: Poster Session B: Liver: Hepatocellular Carcinoma and Other Malignancies
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Primary liver sarcomas (PLS) are rare tumors and encompass subtypes with diverse histology and varying outcomes. These subtypes include embryonal sarcoma (ES), rhabdomyosarcoma (RMS), and unclassified primary liver sarcoma (U-PLS). Malignant rhabdoid tumor of the liver (MRT), first described in 2004, is a new, distinct subcategory of PLS characterized by absence of nuclear INI1 protein staining, and loss of function mutations in the corresponding SMARB1 gene on chromosome 22.
Liver transplantation (LT) can provide definitive cure for unresectable PLS. However, survival outcomes after LT for these extremely rare tumors are poorly understood. Our aim was to analyze outcomes after LT for PLS in United States (US) over last three decades.
*Methods: The outcomes of 29 children with PLS, who received LT between 1988-2018 in the US were queried from the Scientific Registry for Transplant Recipients (SRTR). No LT were recorded for MRT before the year 2000. Therefore, children were grouped into Era 1 (1988-1999) and Era 2 (2000-18).
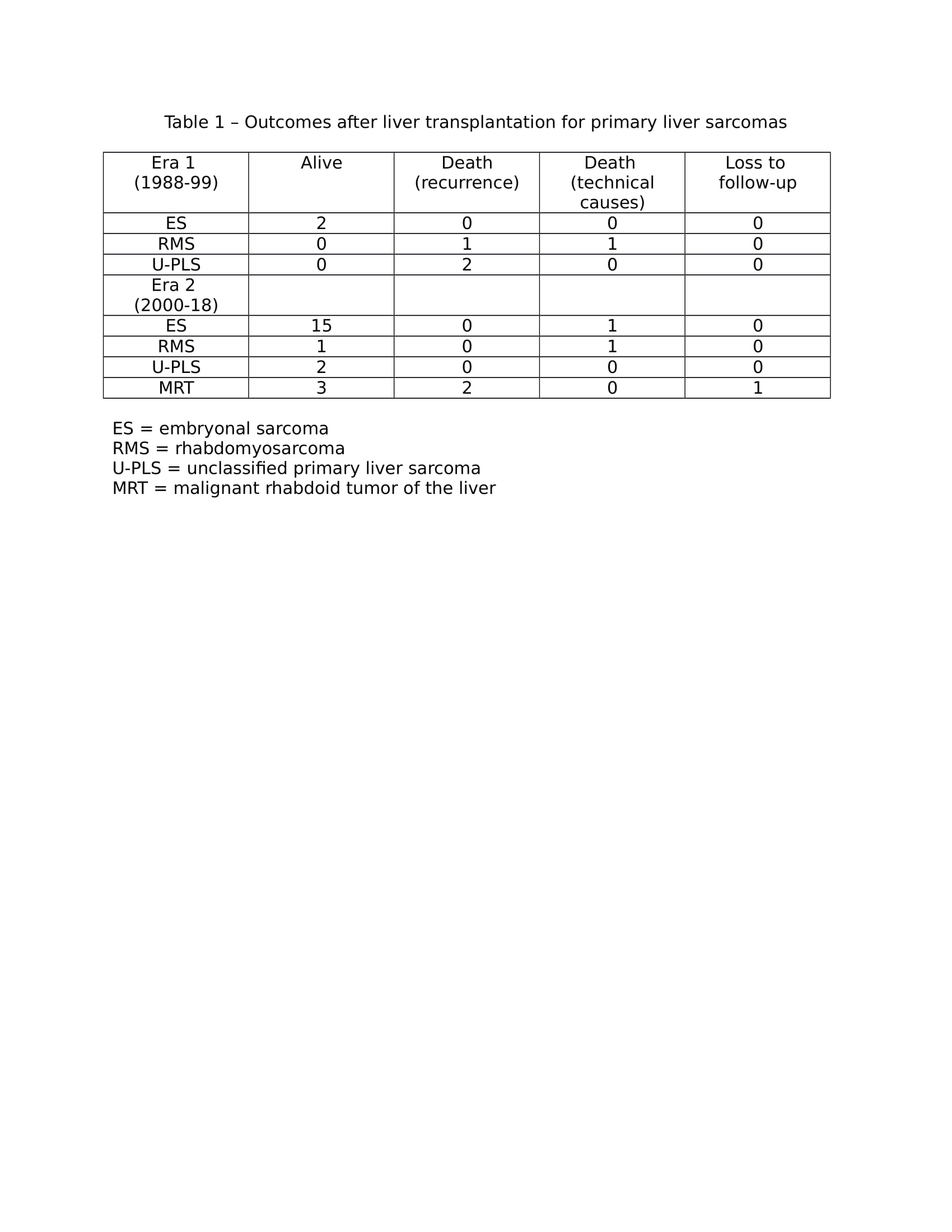
*Results: Median age was 9 years (range 1 – 17), and median follow-up was 388 days (range 0 to 5713). The distribution of males: females was 12 : 17, Caucasian: African-American: others was 21 : 7 : 1, cadaveric: living donor grafts was 24 : 5, and segmental: whole liver grafts was 9 : 20. Ten-year patient survival after LT for ES was 99% vs 94% (p=NS) in Era 1 (n=2) vs Era 2 (n=16), respectively, p=NS. Ten-year patient survival for RMS and U-PLS as a group, improved significantly from 0% in Era 1 (n=4) to 75% in Era 2 (n=4), p=0.036. Post-transplant outcomes – alive, death due to recurrence, death due to technical causes or loss to follow-up are shown in Table 1. After LT for ES, both children in Era 1 and 15 of 16 children in Era 2 survived. After LT for RMS or U-PLS, death due to recurrence occurred at a median interval of 111 days (89-1282) in three of four children in Era 1. No recurrence-related deaths occurred in Era 2. Two of three children with MRT died of recurrence at 200 and 256 days after LT. The outcome of the third child with MRT is not recorded past the day of LT.
*Conclusions: Patient survival remains excellent after LT for unresectable ES in children. Recurrence-free survival after LT for RMS and U-PLS has been excellent in the last two decades compared with the previous era, likely because of better patient selection. Fatal recurrences are most common after LT for MRT and must be undertaken with a better understanding of tumor biology.
To cite this abstract in AMA style:
Amin A, Soltys K, Ranganathan S, Bond G, Khanna A, Ganoza A, Sun Q, Mazariegos G, Sindhi R. Liver Transplantation for Primary Liver Sarcoma in Children-The US Experience from the Scientific Registry for Transplant Recipients (1988-2018) [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/liver-transplantation-for-primary-liver-sarcoma-in-children-the-us-experience-from-the-scientific-registry-for-transplant-recipients-1988-2018/. Accessed March 1, 2026.« Back to 2020 American Transplant Congress