Liver Transplantation for Patients with Cholangiocarcinoma: A Systematic Review and Meta-Analysis of Survival Rates
I. A. Ziogas1, K. P. Economopoulos2, M. H. Hayat1, L. K. Matsuoka1, M. I. Montenovo1, M. Izzy1, S. P. Alexopoulos1
1Vanderbilt University Medical Center, Nashville, TN, 2Duke University Medical Center, Durham, NC
Meeting: 2020 American Transplant Congress
Abstract number: 254
Keywords: Liver transplantation, Malignancy, Meta-analysis
Session Information
Session Name: Liver: Hepatocellular Carcinoma and Other Malignancies II
Session Type: Oral Abstract Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:45pm
 Presentation Time: 4:03pm-4:15pm
Presentation Time: 4:03pm-4:15pm
Location: Virtual
*Purpose: Liver transplant (LT) accompanied by neoadjuvant chemoradiation has emerged as the only curative option for unresectable cholangiocarcinoma (CCA). Although numerous centers have published their outcomes after LT for patients with intrahepatic or hilar CCA, no recent quantitative assessment of the survival outcomes has been attempted. We aimed to perform a meta-analysis of the survival outcomes for patients with CCA after LT.
*Methods: A systematic literature search of the PubMed and Cochrane databases was performed with respect to the PRISMA statement (end-of-search date: September 24th, 2019). Meta-analysis of proportions for overall survival (OS) and overall recurrence rates was performed using the random-effects model.
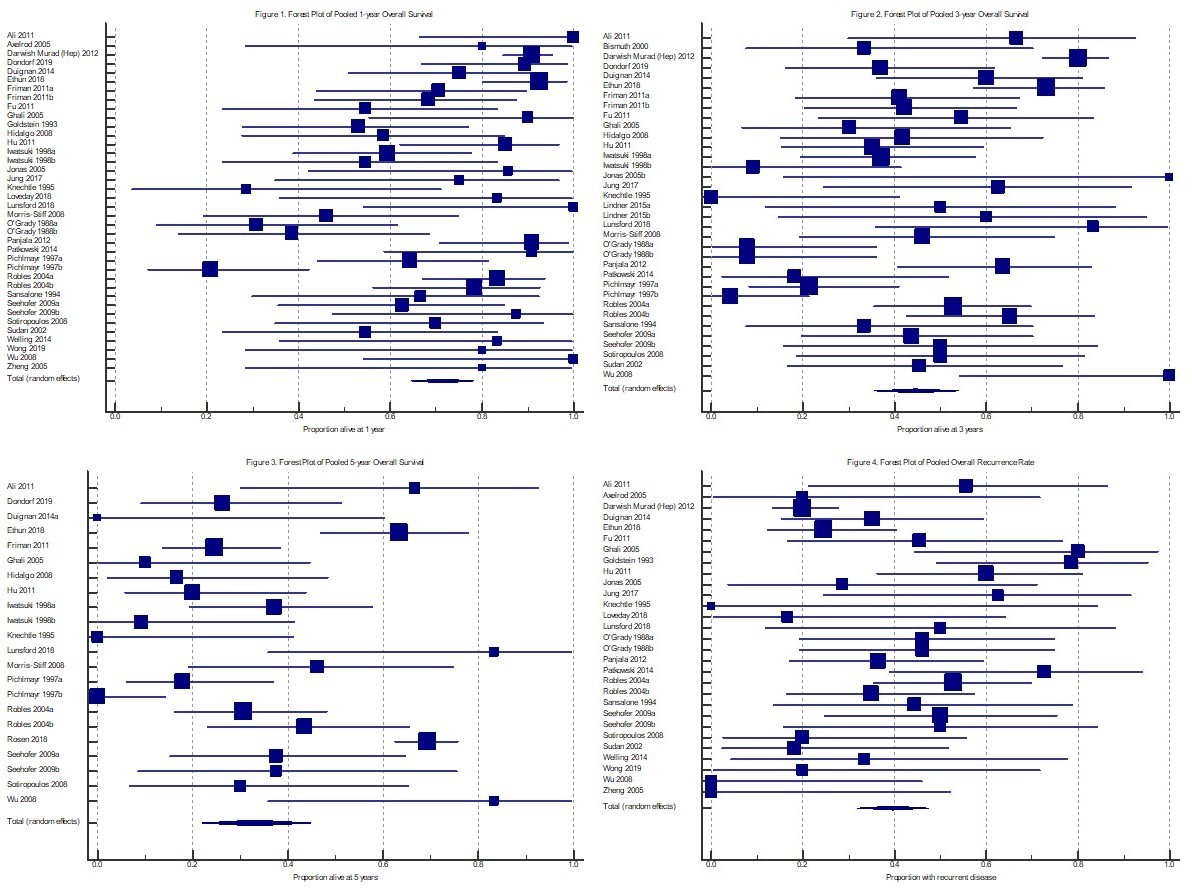
*Results: 37 non-overlapping original articles reporting on a total of 819 patients were included. 68.3% (n=285/417) were male, 47.2% (n=331/701) had underlying primary sclerosing cholangitis and 81.4% (n=592/727) of the patients were known to have CCA before LT (non-incidental) while 18.6% (n=135/727) of the patients were diagnosed with CCA on explant pathology (incidental). 30.2% (n=237/785) of the tumors were intrahepatic, and 69.8% (n=548/785) were hilar. 85.3%, 14% and 0.7% of the patients underwent deceased donor, living donor and domino LT, respectively, and 16.8% of the patients underwent Whipple’s procedure along with the LT. The pooled 1-, 3-, and 5-year OS rates were 71.6% (95%CI: 64.5-78.1; I2=73%, P<0.0001; Figure 1), 44.5% (95%CI: 35.4-53.8; I2=81.4%, P<0.0001; Figure 2), and 32.9% (95%CI: 21.9-44.9; I2=87.4%, P<0.0001; Figure 3), respectively. The pooled overall recurrence rate was 39.5% (95%CI: 31.9-47.4; I2=63.9%, P<0.0001; Figure 4).
*Conclusions: LT has been broadly utilized for CCA patients worldwide. With only one-third of the patients surviving more than 5 years, more careful utilization of LT for CCA is warranted to improve these poor outcomes.
To cite this abstract in AMA style:
Ziogas IA, Economopoulos KP, Hayat MH, Matsuoka LK, Montenovo MI, Izzy M, Alexopoulos SP. Liver Transplantation for Patients with Cholangiocarcinoma: A Systematic Review and Meta-Analysis of Survival Rates [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/liver-transplantation-for-patients-with-cholangiocarcinoma-a-systematic-review-and-meta-analysis-of-survival-rates/. Accessed March 7, 2026.« Back to 2020 American Transplant Congress