Is Low Systemic Fibrinolytic Activity During the Anhepatic Phase Liver Transplant Surgery Associate with the Dreaded Post-Operative Complication of Hepatic Artery Thrombosis?
H. B. Moore1, Y. Bababekov1, J. Pomposelli1, T. Ferrell1, F. Azam1, M. Adams2, D. Yoeli1, R. Choudhury1, M. Wachs2, E. Pomfret1, T. Nydam1
1University of Colorado, Aurora, CO, 2Childrens Hospital Colorado, Aurora, CO
Meeting: 2021 American Transplant Congress
Abstract number: 1131
Keywords: Graft failure, Liver, Liver transplantation, Living-related liver donors
Topic: Clinical Science » Liver » Liver: Living Donor Liver Transplant and Partial Grafts
Session Information
Session Name: Liver: Living Donor Liver Transplant and Partial Grafts
Session Type: Poster Abstract
Session Date & Time: None. Available on demand.
Location: Virtual
*Purpose: Removal of the native liver during transplantation results in impaired clearance of clot degrading proteins and activation of fibrinolysis as appreciated by Starzl in the 1960s. Hypofibrinolysis (lack of activation of the fibrinolytic system when anticipated) has been associated with thrombotic complications in non-transplant patients. Hypofibrinolysis in liver transplantation has not previously been evaluated, and would be presumed to increase the risk of hepatic artery thrombosis (HAT), particularly in living donor grafts or when arterial reconstruction is needed in cadaveric donors. We hypothesize that hypofibrinolysis during the anhepatic phase of surgery would be associated with an increased risk of HAT.
*Methods: Consenting adult liver transplant recipients underwent a research thrombelastography (TEG) 15-minutes after portal vein ligation (anhepatic) to evaluate systemic fibrinolytic activity. Fibrinolysis activity was quantified by the amount of clot strength lost from peak clot strength in 30-minutes (LY30). A receiver operating characteristic curve (ROC) was used to identify a threshold for hepatic artery thrombosis (HAT) using the Youden index with the anheptic TEG LY30. Patient with the need for hepatic arterial reconstruction or received a living donor graft were classified as increased risk of thrombosis(IRT).
*Results:
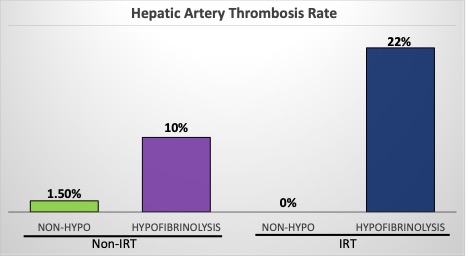
130 liver transplant patient recipients with a median laboratory na-MELD of 22 on the day of surgery were included in the analysis. IRT was present in 14%. HAT occurred in 5% of patients in which the rate was doubled in the IRT group (11%). The ROC Youden index identified a LY30 of <1% as a predictor of HAT (which defined hypofibrinolysis). Hypofibrinolysis was detected in 38% of patients. HAT occurred in 12% of patients with hypofibrinolysis vs 1.5% of patients that generated a fibrinolytic response (p=0.015). Patients with IRT and hypofibrinolysis had a 22% rate of HAT vs 0% in those that generated a fibrinolytic response (Figure). This same elevated HAT rate in hypofibrinolysis was also seen in patient with normal risk vascular anastomoses (10% hypo vs 1.5% Figure).
*Conclusions: Hypofibrinolysis (anhepatic TEG LY30 < 1%) predicts increased risk of HAT. Attenuating HAT warrants further work to understand both mechanisms behind these findings and evaluating interventions, while avoiding excessive bleeding risk.
To cite this abstract in AMA style:
Moore HB, Bababekov Y, Pomposelli J, Ferrell T, Azam F, Adams M, Yoeli D, Choudhury R, Wachs M, Pomfret E, Nydam T. Is Low Systemic Fibrinolytic Activity During the Anhepatic Phase Liver Transplant Surgery Associate with the Dreaded Post-Operative Complication of Hepatic Artery Thrombosis? [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/is-low-systemic-fibrinolytic-activity-during-the-anhepatic-phase-liver-transplant-surgery-associate-with-the-dreaded-post-operative-complication-of-hepatic-artery-thrombosis/. Accessed February 17, 2026.« Back to 2021 American Transplant Congress