Intra-Abdominal Hypertension in Simultaneous Pancreas-Kidney Transplantation
Nephrology and Transplantation, Guy's and St Thomas' NHS Foundation Trust, London, United Kingdom
Meeting: 2019 American Transplant Congress
Abstract number: D283
Keywords: Graft function, Ischemia, Post-operative complications, Risk factors
Session Information
Session Name: Poster Session D: Pancreas and Islet: All Topics
Session Type: Poster Session
Date: Tuesday, June 4, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall C & D
*Purpose: There have been several reports of raised intra-abdominal pressure (IAP) in solid organ transplantation, including life threatening abdominal compartment syndrome requiring decompressive laparotomy. In simultaneous pancreas-kidney transplants (SPK) however, it remains unknown whether IAP increases and if so to what extent. We conducted a pilot study to explore the incidence of intra-abdominal hypertension (IAH) and risk factors in SPKs.
*Methods: A prospective cohort study was undertaken in adult SPKs performed at our centre during the 6-month study period. Preoperative and postoperative IAPs along with other clinically relevant transplant-specific variables were recorded over the first 3 postoperative days (POD). Clinical outcomes were monitored for a period of 3 months. Matched pair and univariate regression analyses were performed to explore the incidence of IAH and identify possible risk factors.
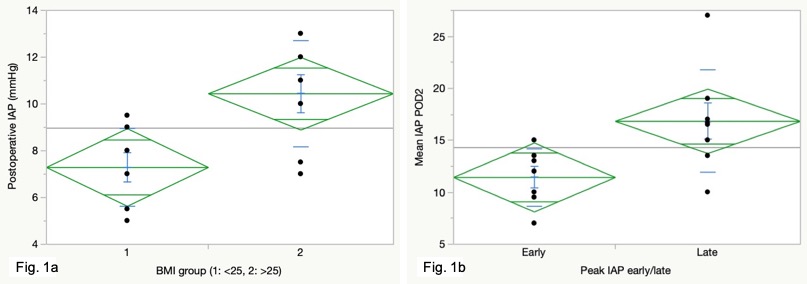
*Results: 15 consecutive SPKs (11 DBD and 4 DCD) were analysed. The mean IAPs at baseline, immediately postoperative, POD1, POD2 and POD3 were 5.4, 8.9, 11.0, 14.3 and 12.5 mmHg, respectively. Throughout the study, all patients had a clinically gradable IAH: 36% of patients sustained grade 1, while 64% of patients sustained grade 2 to 4 IAH. Matched pair analysis demonstrated a statistically significant rise in IAP in the immediate postoperative period by a mean 3.5 mmHg (p <0.0001). In addition to this, the peak postoperative IAP was significantly higher than the immediate postoperative IAP by a mean 9.6 mmHg (p <0.0001). Postoperative IAPs were significantly higher in the higher recipient BMI group (BMI>25) compared to the lower recipient BMI group (<25) (Fig. 1a). Patients with late onset (>48 hrs) IAH had significantly higher mean IAP as compared to those with early onset (<48 hrs) IAH (p=0.02) (Fig. 1b). Interestingly, longer pancreas cold ischemia time was associated with higher IAP on POD2 (p >0.02). This pilot study was expectedly underpowered for correlation with adverse clinical outcomes. All pancreas and kidney grafts were functioning at 1 and 3 months.
*Conclusions: This is the first study to establish an association between SPK transplantation and IAH, which could have potentially detrimental effects on graft function and survival. Increasing the sample size to explore clinical implications of IAH would be best done within a multi-centre study. In view of our findings, we suggest routine IAP measurement is integrated in clinical practice in SPK transplantation.
To cite this abstract in AMA style:
Ameen T, Papadakis G, Punjala R, Karydis N. Intra-Abdominal Hypertension in Simultaneous Pancreas-Kidney Transplantation [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/intra-abdominal-hypertension-in-simultaneous-pancreas-kidney-transplantation/. Accessed July 9, 2025.« Back to 2019 American Transplant Congress