Inflammation and Fibrosis Are Observed in 34% of Clinically Stable Adult Liver Transplant Recipients
1ITN, San Francisco, CA, 2Northwestern, Chicago, IL, 3UCSF, San Francisco, CA, 4UPMC, Pittsburg, PA, 5Columbia, New York, NY, 6UPenn, Philadelphia, PA, 7Baylor, Dallas, TX, 8Rho, Chapel Hill, NC, 9NIAID, Bethesda, MD, 10ITN, Bethesda, MD, 11MGH, Boston, MA
Meeting: 2019 American Transplant Congress
Abstract number: D353
Keywords: Biopsy, Liver, Liver transplantation, Screening
Session Information
Session Name: Poster Session D: Tolerance: Clinical Studies
Session Type: Poster Session
Date: Tuesday, June 4, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall C & D
*Purpose: OPTIMAL is a 7-center immunosuppression withdrawal (ISW) study in non-autoimmune, non-HCV adult liver transplant recipients ≥3 yrs post-transplant (tx) (NCT02533180). Subjects underwent a screening liver biopsy to exclude unfavorable histology and potentially identify tissue biomarkers of tolerance.
*Methods: 91 biopsies have been performed. Histologic inclusion criteria are noted in Table 1. Histologically eligible and ineligible subjects were compared using Fisher’s exact or Wilcoxon rank sum tests.
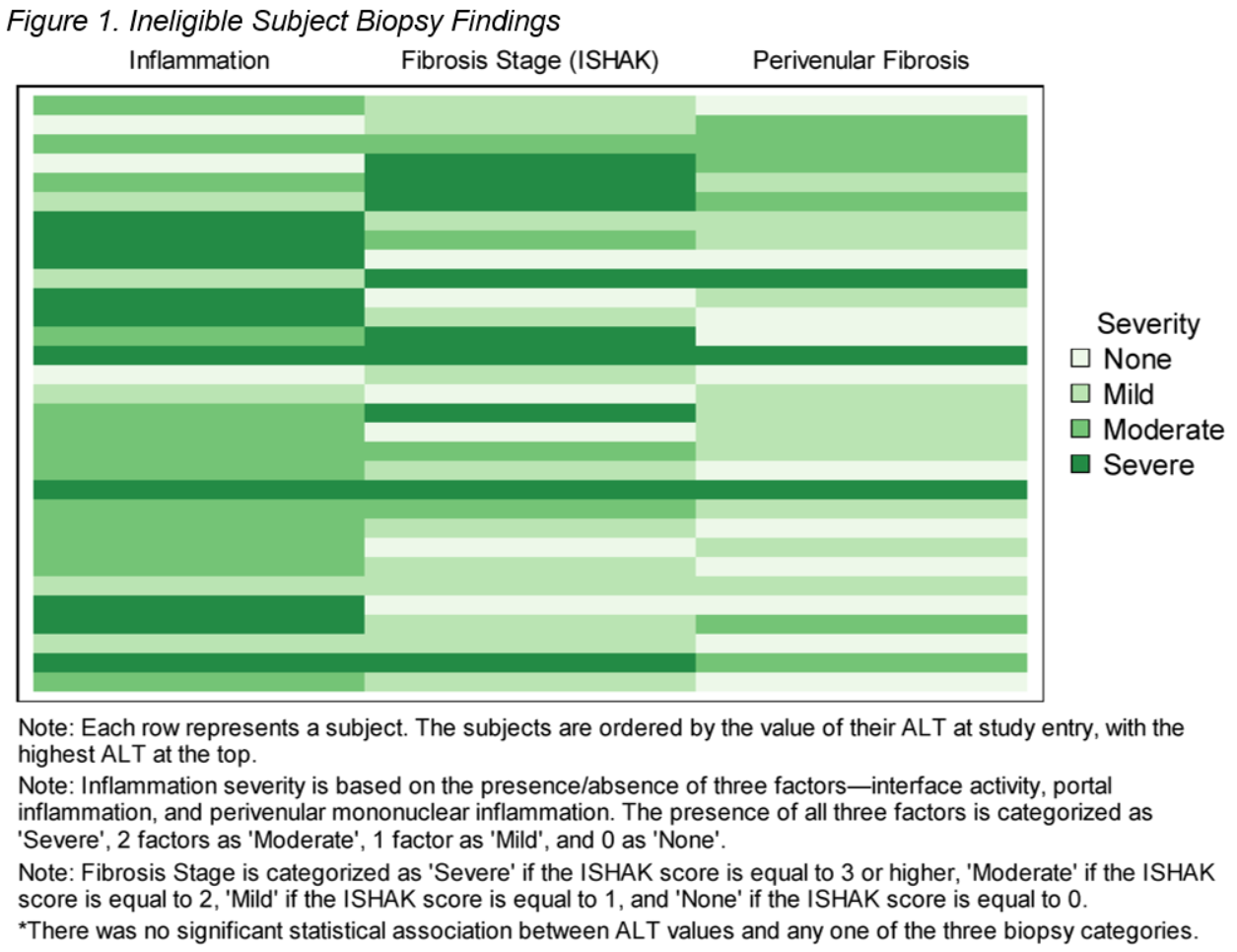
*Results: 31/91 subjects were ineligible due to inflammation (n=17) and/or fibrosis (n=9), or bile duct damage (n=3), or arteriopathy (n=3). Figure 1 shows the distribution of inflammation and fibrosis in the ineligible subjects. No significant differences were observed between the 2 groups in terms of liver failure cause/sex/race, IS type, time post-tx, ALT/GGT, or donor type/age/sex (Table 2). Eligible subjects were significantly older at tx (56 vs. 48) and enrollment (64 vs. 54), and had a higher frequency of steatohepatitis (52% vs. 10%).
*Conclusions: 1/3 of biopsies from long-term, stable liver transplant recipients harbored subclinical inflammation and/or fibrosis. Increased recipient age at tx and enrollment, but not time from tx, correlated with histologic eligibility. Eligible biopsies were also more likely to have steatohepatitis. The natural history and significance of these biopsy findings is unknown. We plan to further analyze correlations of these observations with study outcomes.
To cite this abstract in AMA style:
Sun L, Levitsky J, Feng S, Humar A, Demetris AJ, Emond J, Shaked A, Klintmalm G, Mason K, DesMarais M, Priore A, Bridges N, Burrell BE, Chandran S, Markmann J. Inflammation and Fibrosis Are Observed in 34% of Clinically Stable Adult Liver Transplant Recipients [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/inflammation-and-fibrosis-are-observed-in-34-of-clinically-stable-adult-liver-transplant-recipients/. Accessed February 17, 2026.« Back to 2019 American Transplant Congress