Impact of Donation After Circulatory Death Donor Allografts on Outcomes Following Liver Transplantation for Cholangiocarcinoma
1Digestive Disease Institute, Cleveland Clinic Abu Dhabi, Abu Dhabi, United Arab Emirates, 2Department of Quantitative Health Sciences, Cleveland Clinic Foundation, Cleveland, OH
Meeting: 2021 American Transplant Congress
Abstract number: 1115
Keywords: Bile duct, Donors, non-heart-beating, Liver transplantation, Malignancy
Topic: Clinical Science » Liver » Liver: Hepatocellular Carcinoma and Other Malignancies
Session Information
Session Name: Liver: Hepatocellular Carcinoma and Other Malignancies
Session Type: Poster Abstract
Session Date & Time: None. Available on demand.
Location: Virtual
*Purpose: Improvements in the management of extra-hepatic cholangiocarcinoma (CCA) resulted in allocation of a standardized model for end-stage liver disease (MELD) exception score for liver transplantation (LT) in 2009 for selected patients who completed an approved neoadjuvant chemoradiation protocol. Limited data exists regarding donation after circulatory death (DCD) grafts in CCA despite higher reported incidence of biliary complications. We compared outcomes following DCD LT in CCA (DCD-CCA) with deceased donor (DBD-CCA) and living donor LT (LDLT-CCA), as well as DCD in Hepatocellular carcinoma (DCD-HCC) and indications other than HCC or CCA (DCD-non-CCA/HCC).
*Methods: Using SRTR, retrospective study cohorts were constructed over the time period 2009-2019. Primary outcome measures were graft and patient survival. A chi-square test was used for categorical and Student’s t-test for continuous variables. Survival comparison was performed using the Kaplan-Meier method with log-rank test and multivariable analysis of outcomes using Cox proportional hazard models.
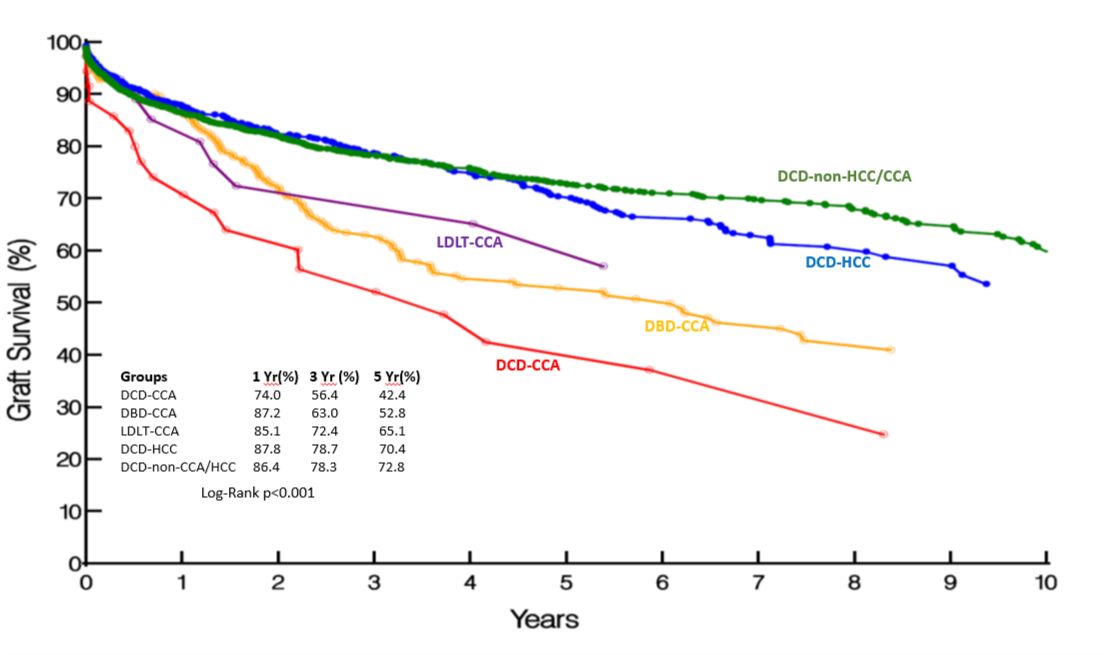
*Results: 425 recipients underwent LT for CCA over the study period: DCD-CCA: 36 (8.5%), DBD-CCA: 361 (85%), LDLT-CCA: 28 (6.5%). 884 and 3101 recipients respectively underwent DCD-HCC and DCD-non-CCA/HCC. All CCA groups were comparable with respect to donor, recipient variables, cold ischemia time (except LDLT-CCA) and time from listing to LT. Mean lab MELD in DCD-CCA was lower than DBD-CCA (12.9 vs 14.3, p=0.02) and DCD-non-CCA/HCC (12.9 vs 19.6; p<0.0001), but comparable to DCD-HCC (12.9 vs 13; p=0.27). Observed graft survival in DCD-CCA was lower than DBD-CCA and LDLT-CCA (Fig 1). However patient survival in the 3 CCA groups was comparable: DCD-CCA, DBD-CCA, LDLT-CCA (%): 1 Yr: 82.2 vs 89.2 vs 88.7; 3 Yr: 64.4 vs 65.1 vs 75.4; 5 Yr: 55.8 vs 55.1 vs 67.9 (p=0.44). Outcomes in DCD-CCA were also inferior to DCD-HCC and DCD-non-CCA/HCC. On multivariable analysis, while cold ischemia time was predictive of both graft and patient survival in CCA, recipient DCD status was only predictive of graft (HR (95% CI): 1.69 (1.03-2.76), p=0.03), but not patient survival (HR (95% CI): 1.39 (0.81-2.37), p=0.22).
*Conclusions: Even though graft survival following DCD LT in CCA is inferior to DBD and LDLT, patient survival is comparable. Consideration of DCD in CCA may confer a survival advantage when weighed against likelihood of wait-list drop out in carefully selected recipients with a time-sensitive need for LT.
To cite this abstract in AMA style:
Kumar S, Lin S, Schold JD. Impact of Donation After Circulatory Death Donor Allografts on Outcomes Following Liver Transplantation for Cholangiocarcinoma [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/impact-of-donation-after-circulatory-death-donor-allografts-on-outcomes-following-liver-transplantation-for-cholangiocarcinoma/. Accessed February 26, 2026.« Back to 2021 American Transplant Congress