Human Urine-Derived Stem Cells Protect Renal Function by Releasing miR-129-5p Which Targets High-Mobility Group Box-1 (HMGB1) in Rat Ischemia Reperfusion Injury Model
Organ Transplant Center, The First Affiliated Hospital of Sun Yet-sen University, New York, NY, China.
Meeting: 2018 American Transplant Congress
Abstract number: B14
Keywords: Inflammation, Renal injury, Renal ischemia, Stem cells
Session Information
Session Name: Poster Session B: Acute and Chronic Graft Injury
Session Type: Poster Session
Date: Sunday, June 3, 2018
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
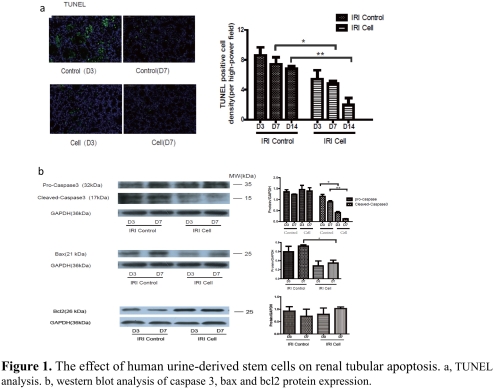
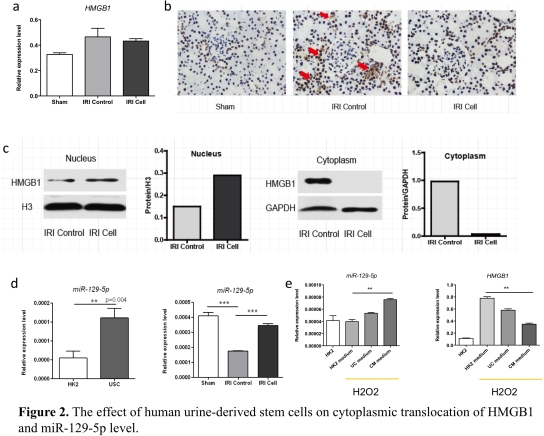
Location: Hall 4EF
Objective: This study investigated the protective effect of human urine-derived stem cells (USCs) on renal ischemia reperfusion injury (IRI) in rats. Methods: Human USCs was cultured and harvested from fresh spot urine. Left renal pedicles was occluded for 45 minutes to induce renal IRI model in rats. Human USCs (2*106 cells) was intravenously administered right after blood reperfusion. Results: Compared to the control, human USCs significantly increased rat survival rate (p=0.03), and decreased serum creatinine and blood urine nitrogen (BUN)(p<0.05). Acute tubular injury score was significantly decreased in USCs group (p=0.03). TUNEL analysis showed fewer apoptotic cells in USCs group (Fig. 1a, p<0.05). The cleaved-caspase 3 and bax were decreased while bcl2 was increased in USCs group (Fig. 1b, p<0.05). Myeloperoxidase (MPO) staining score was significantly lower in USCs group (p<0.05). Notably, the releasing of HMGB1 from nucleus was significantly decreased in USCs group (Fig. 2b,2c), while its mRNA expression level in total renal tissue was similar to the control (Fig. 2a). Meanwhile, miR-129-5p expression in renal tissue was significantly unregulated in USCs group (Fig. 2d). In an oxidative-stressed HK2 cell culture model, USCs conditioned medium significantly increased miR-129-5p level while reduced HMGB1 (Fig. 2e). Discussion and Conclusion: Our data demonstrated that human USCs attenuate renal ischemia reperfusion injury in rats. By bioinformatics analysis, we found miR-129-5p could target HMGB1 and reduce HMGB1 level. We hypothesize human USCs inhibits the expression and releasing of HMGB1 in injury renal tubular cells probably through the release of miR-129-5p and subsequently inhibit infiltration of inflammatory cells.
CITATION INFORMATION: Liu L., Li X., Su Q., Bi Z., Huang H., Wang C. Human Urine-Derived Stem Cells Protect Renal Function by Releasing miR-129-5p Which Targets High-Mobility Group Box-1 (HMGB1) in Rat Ischemia Reperfusion Injury Model Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Liu L, Li X, Su Q, Bi Z, Huang H, Wang C. Human Urine-Derived Stem Cells Protect Renal Function by Releasing miR-129-5p Which Targets High-Mobility Group Box-1 (HMGB1) in Rat Ischemia Reperfusion Injury Model [abstract]. https://atcmeetingabstracts.com/abstract/human-urine-derived-stem-cells-protect-renal-function-by-releasing-mir-129-5p-which-targets-high-mobility-group-box-1-hmgb1-in-rat-ischemia-reperfusion-injury-model/. Accessed February 17, 2026.« Back to 2018 American Transplant Congress