Human Leukocyte Antigen Class I (HLA-I) Antibodies in Patients Undergoing Liver Transplantation: Implications for Platelet Transfusion Support
1Div. of Transplant Surgery, Medical College of Wisconsin, Milwaukee, WI, 2Div. of Hematology/Oncology, Medical College of Wisconsin, Milwaukee, WI, 3Medical College of Wisconsin and BloodCenter of Wisconsin, Milwaukee, WI
Meeting: 2019 American Transplant Congress
Abstract number: A137
Keywords: Alloantibodies, HLA matching, Liver, Thrombocytopenia
Session Information
Session Name: Poster Session A: Biomarkers, Immune Monitoring and Outcomes
Session Type: Poster Session
Date: Saturday, June 1, 2019
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Hall C & D
*Purpose: Liver transplantation is a high platelet transfusion (PLT) setting due to the elevated incidence of thrombocytopenia and bleeding. HLA-I antibodies are thought to have no major impact on liver allograft function, however, platelets express HLA-I antigens and it is not known if these antibodies can mediate refractoriness to PLT in this setting. This study sought to examine the effect of HLA-I antibodies on PLT refractoriness in liver transplantation.
*Methods: We retrospectively reviewed peritransplant clinical and PLT factors for all adult liver or liver-kidney transplants (SLK) performed at our center between October 2012 and September 2017. Sensitized patients (SE) with pre-transplant HLA-I calculated panel-reactive antibody (cPRA) ≥20% were compared to unsensitized patients (US) with cPRA <20%. Mean follow up was 21.4 months.
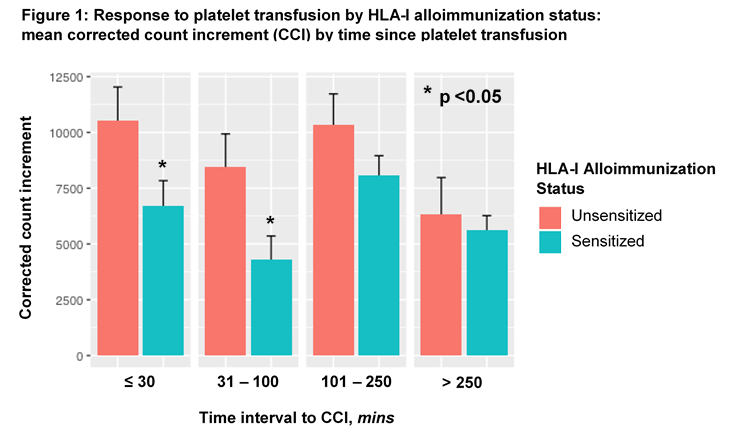
*Results: Alloimmunization was observed in 39% of the study cohort. SE (n=28) received 272 PLTs (256 unmatched, 16 matched units), and US (n=44) received 246 unmatched PLTs. History of pregnancy was higher among SE than US (p <0.01); otherwise both groups had similar clinical characteristics. SE had higher rates of PLT refractoriness compared to US, defined as a platelet corrected count increment (CCI) <7500 at ≤1 hour after transfusion (66% vs 42%, p <0.001). Mean CCI was lower among SE compared to US immediately after PLT (6713 vs 10541, p <0.05, Fig 1), a critical time for attaining hemostasis. SE also tended to receive more PLTs than US (p <0.07). Alloimmunization and SLK were independent predictors of refractoriness on multivariate logistic regression (p <0.05). While posttransplant length of stay was significantly longer for SE (p<0.01), early rejection, patient and graft survival at discharge, and overall patient survival did not differ between groups.
*Conclusions: Patients undergoing liver transplantation experienced high rates of HLA-I alloimmunization and PLT refractoriness, as evidenced by significantly lower CCIs. Our study suggests that HLA-matched PLT in HLA-I alloimmunized patients, a standard practice in areas such as oncology, may mitigate PLT refractoriness in liver transplant patients. While SE tended to need more PLT and have longer hospitalization, early and late outcomes were not affected.
To cite this abstract in AMA style:
Wong M, Narra R, Selim M, Zimmerman MA, Padmanabhan A, Hong JC. Human Leukocyte Antigen Class I (HLA-I) Antibodies in Patients Undergoing Liver Transplantation: Implications for Platelet Transfusion Support [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/human-leukocyte-antigen-class-i-hla-i-antibodies-in-patients-undergoing-liver-transplantation-implications-for-platelet-transfusion-support/. Accessed February 19, 2026.« Back to 2019 American Transplant Congress