Histologic Ischemia Reperfusion Injury in Liver Transplantation: A Large Single Center Experience
Department of Surgery, The Dumont-UCLA Transplant Center, Los Angeles, CA
Meeting: 2019 American Transplant Congress
Abstract number: 98
Keywords: Biopsy, Ischemia, Liver grafts, Liver transplantation
Session Information
Session Name: Concurrent Session: Non-Organ Specific:Organ Preservation/Ischemia Reperfusion Injury
Session Type: Concurrent Session
Date: Sunday, June 2, 2019
Session Time: 2:30pm-4:00pm
 Presentation Time: 2:54pm-3:06pm
Presentation Time: 2:54pm-3:06pm
Location: Room 209
*Purpose: Ischemia Reperfusion Injury (IRI) is known to adversely affect graft outcomes in Liver Transplantation (LT). Large series examining the significance of IRI found on Intraoperative Post Reperfusion Biopsies (IPRB) remain limited. This is of renewed significance as the transplant community continues to push the envelope on the use of marginal donors to expand the donor pool. This study sought to examine the incidence, severity, and predictors of IRI found on IPRB and assess its impact on graft outcomes.
*Methods: IPRB were collected approximately 2 hours after reperfusion during LT. IRI was graded and compared based on histological findings: no IRI, minimal, mild, moderate, and severe. Pre and intraoperative risk factors for IRI and early allograft dysfunction (EAD) were identified using multivariate logistic regression. Graft failure was defined as patient death or re-LT. (492 LT’s, retrospective review, single academic center, 2012 – 2017).
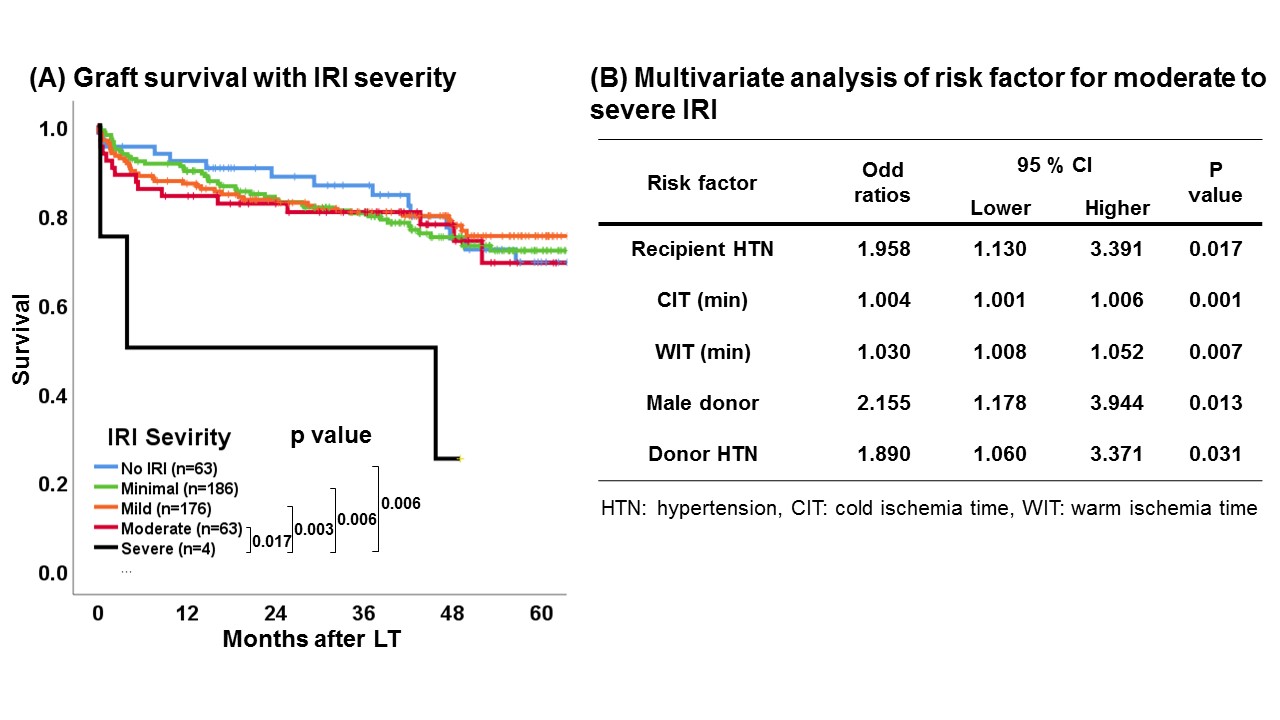
*Results: Of 492 LT’s, 49.4% had mild or more IRI (no IRI: 12.8%, minimal: 37.8%, mild: 35.8%, moderate: 12.8%, severe: 0.8%). Increased IRI severity correlated with increased graft failure rates at 6 months (no IRI: 4.8%, minimal: 8.1%, mild: 11.4%, moderate: 14.3%, severe: 50.0%, p<0.05). Grafts with severe IRI had significantly poorer long term outcomes (Figure A). Independent risk factors for moderate to severe IRI were longer cold ischemia time (OR: 1.004, p=0.001), longer warm ischemia time (OR: 1.958, p=0.007), recipient hypertension (OR: 1.958, p=0.017), donor hypertension (OR: 1.890, p=0.031), and male donors (OR: 2.155, p=0.031) (Figure B). Moderate to severe IRI was associated with higher rates of EAD (40.3% vs 24.2%, p<0.01), and was an independent risk factor for its incidence (OR: 2.251, p=0.009).
*Conclusions: This represents one of the largest reports examining the correlation between IPRB results and outcomes in LT. While increased IRI severity correlated with inferior short term graft outcomes, only severe IRI was associated with worse long term outcomes. We identified 5 risk factors (cold ischemia time, warm ischemia time, recipient hypertension, donor hypertension, and male donors) for moderate to severe IRI. Careful consideration of these factors during donor-recipient matching may assist in optimizing graft utilization and LT outcomes.
To cite this abstract in AMA style:
Kaldas FM, Ito T, Younan S, Aziz J, Lu M, Agopian VG, III JDiNorcia, Yersiz H, Farmer DG, Busuttil RW. Histologic Ischemia Reperfusion Injury in Liver Transplantation: A Large Single Center Experience [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/histologic-ischemia-reperfusion-injury-in-liver-transplantation-a-large-single-center-experience/. Accessed February 15, 2026.« Back to 2019 American Transplant Congress