Graft Survival after Liver Transplantation for Patients with Cholangiocarcinoma
Vanderbilt University Medical Center, Nashville, TN
Meeting: 2020 American Transplant Congress
Abstract number: 250
Keywords: Graft survival, Liver transplantation, Malignancy, N/A
Session Information
Session Name: Liver: Hepatocellular Carcinoma and Other Malignancies II
Session Type: Oral Abstract Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:45pm
 Presentation Time: 3:15pm-3:27pm
Presentation Time: 3:15pm-3:27pm
Location: Virtual
*Purpose: Liver transplantation (LT) with neoadjuvant chemoradiation is increasingly utilized for the treatment for unresectable cholangiocarcinoma (CCA), however, post-LT graft survival is not well described. We aimed to assess the impact of patient characteristics (age, incidental [listed for other diagnoses but CCA found on explant pathology] vs. non-incidental [listed for CCA and CCA found on explant pathology] diagnosis, deceased donor[DD] vs. living donor[LD], waiting time, laboratory MELD and exception status) and OPTN region on post-LT graft survival in CCA patients.
*Methods: 844 patients undergoing primary LT (2002-2019) for incidental or non-incidental CCA were identified in the Scientific Registry of Transplant Recipients database. Graft survival was analyzed using the Kaplan-Meier method with log-rank tests for between-group comparisons. Multivariable Cox proportional hazards regression evaluated the effects of patient characteristics and OPTN region on risk of graft failure.
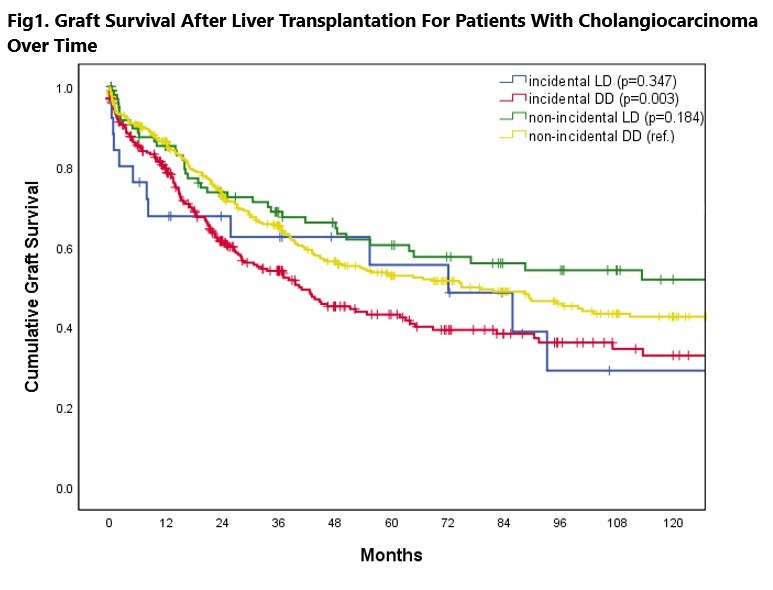
*Results: 100 LDLTs and 432 DDLTs were performed for non-incidental, and 26 LDLTs and 286 DDLTs for incidental CCA. The number of CCA patients transplanted increased over the years (rho=0.85, p<0.001). Overall 1-, and 5-year graft survival rates were 83.1%, and 50.6%, respectively. Unadjusted graft survival for non-incidental DDLT was higher than that of incidental DDLT (p=0.003), with 1-, 5-year rates of 86.2%, 52.8% and 78.9%, 43.1%. Graft survival for non-incidental DDLT did not differ from non-incidental LDLT (p=0.184; 1-year: 85.2%), and it did not differ from incidental LDLT (p=0.347; estimable 1-year: 67.7%) (Fig1). 34.2% of the LTs were performed in region 7. On multivariable analysis, regions 2, 3, 4, 5, 9, and 10 (HR≥1.49, 95%CI: 1.05-3.53, p≤0.03) exhibited increased risk of graft failure while regions 1, 6, 8 and 11 exhibited no difference in risk vs. region 7. Laboratory MELD scores 15-24 (p≤0.04) and ≥40 (p<0.001) were associated with an increased risk of graft failure vs. scores <15. Age, donor type, exception status, waiting time and incidental CCA diagnosis were not associated with risk of graft failure on multivariable analysis.
*Conclusions: Despite the existence of regional differences, the overall 5-year graft survival for patients transplanted with CCA is around 50%. Improvements should be made nationally in the utilization of LT for CCA patients to improve upon this high rate of graft loss.
To cite this abstract in AMA style:
Ziogas IA, Hickman LA, Matsuoka LK, Montenovo MI, Izzy M, Rega SA, Feurer ID, Alexopoulos SP. Graft Survival after Liver Transplantation for Patients with Cholangiocarcinoma [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/graft-survival-after-liver-transplantation-for-patients-with-cholangiocarcinoma/. Accessed March 2, 2026.« Back to 2020 American Transplant Congress