Epithelial To Mesenchymal Transition Mediates Engraftment Of Endoderm And Hepatic Progenitor Cells In The Quiescent Liver
1Surgery, University of Texas Medical Branch, Galveston, TX, 2Surgery, Naiyou Lui, Galveston, TX, 3Ophthalmology, University of Texas Medical Branch, Galveston, TX, 4Pathology, Omar Saldarriaga, Galveston, TX, 5pathology, University of Texas Medical Branch, Galveston, TX, 6Pathology, University of Texas Medical Branch, Galveston, TX
Meeting: 2020 American Transplant Congress
Abstract number: D-317
Keywords: Engraftment, Hepatocytes, N/A, Transcription factors
Session Information
Session Name: Poster Session D: Cellular Therapies, Tissue Engineering / Regenerative Medicine
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Stem cell transplantation to the liver is a promising therapeutic strategy for a variety of disorders. Hepatocyte transplantation has short term efficacy, but can be problematic due to known problems with portal hypertension, inflammation, and sinusoidal thrombosis. We have successfully transplanted small endoderm progenitor cells to reverse a murine model of hemophilia B. Labeling these cells with iron nanoparticles renders them responsive to magnetic fields which can be used to enhance engraftment in the structurally normal mouse liver. However, the mechanisms mediating from the sinusoidal space to the hepatocyte compartment are unknown. We hypothesize that cell migration and invasion is mediated by the progenitor cells’ natural tendency for epithelial to mesenchymal transition (EMT).
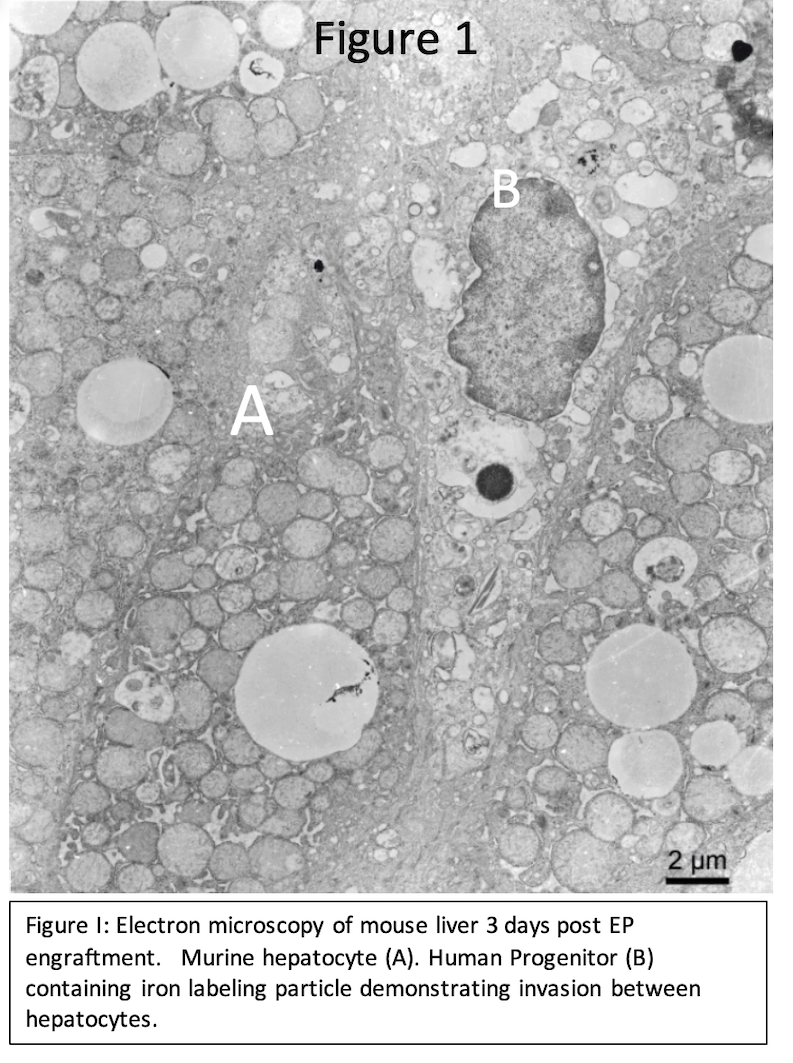
*Methods: Human embryonic stem cells were differentiated to endoderm and hepatic progenitor (EP and HP) cells and confirmed by RT-qPCR and immunofluorescence. These cells were labeled with iron nanoparticles and transplanted to the undamaged liver of immunocompromised or wild-type mice receiving clinical immunosuppression. Early engraftment was analyzed by molecular, histological, and electron microscopy.
*Results: Human EP and HP cells are readily produced with remarkable efficiency. Early timepoint (3h) analysis after transplant to the liver indicate invadeapodia-like structures present, suggesting these cells use EMT for engraftment in the structurally normal quiescent liver. Indeed, in vitro analyses indicate these progenitor cell types are intrinsically biased toward EMT. Analysis 24h after transplant also show extensive migration of EP and HP cells between hepatocytes.
*Conclusions: Early human pluripotent stem cell derivatives demonstrate the cellular mechanism of EMT in vitro and in vivo. This behavior confers on them the ability to engraft via migration from hepatic the sinusoidal space to the hepatocyte space of Disse. This fundamental difference is important for using these cells as a therapeutic for conditions of liver replacement of as a cell-based gene replacement/therapy strategy allowing for safe engraftment without compromise of the organ, which will certainly be important when converting stem cell therapy from the bench to the bedside.
To cite this abstract in AMA style:
Fagg WS, Lui N, Patrikeev L, Saldarriaga* O, Lerner-Stevenson H, Popov V, Motamade M, Fair JH. Epithelial To Mesenchymal Transition Mediates Engraftment Of Endoderm And Hepatic Progenitor Cells In The Quiescent Liver [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/epithelial-to-mesenchymal-transition-mediates-engraftment-of-endoderm-and-hepatic-progenitor-cells-in-the-quiescent-liver/. Accessed February 27, 2026.« Back to 2020 American Transplant Congress