Early Allograft Dysfunction in the Setting of Histologic Ischemia Reperfusion Injury Following Liver Transplantation: Analysis of Predictors and Outcomes
Department of Surgery, The Dumont-UCLA Transplant Center, Los Angeles, CA
Meeting: 2019 American Transplant Congress
Abstract number: D257
Keywords: Biopsy, Graft failure, Ischemia, Liver grafts
Session Information
Session Name: Poster Session D: Non-Organ Specific:Organ Preservation/Ischemia Reperfusion Injury
Session Type: Poster Session
Date: Tuesday, June 4, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall C & D
*Purpose: Hepatic ischemia-reperfusion injury (IRI) in Liver Transplantation (LT) is believed to contribute to Early Allograft Dysfunction (EAD). However, the relationship between IRI and EAD remains unclear. We sought to examine graft outcomes and identify predictors of EAD.
*Methods: The grade of IRI was determined by histological findings (none, minimal, mild, moderate, and severe). EAD was defined as a peak aminotransferase value >2000 IU/mL during the first week post LT, an INR of ≥1.6, or bilirubin ≥10 mg/dL at day 7. Mild to severe IRI (MSIRI) grafts were divided into two groups based on the occurrence of EAD. Risk factors of EAD in patients with IRI on post reperfusion liver biopsy were identified using multivariate logistic regression. Graft survival was compared using Log rank test. (492 adult LT’s, retrospective review, single center).
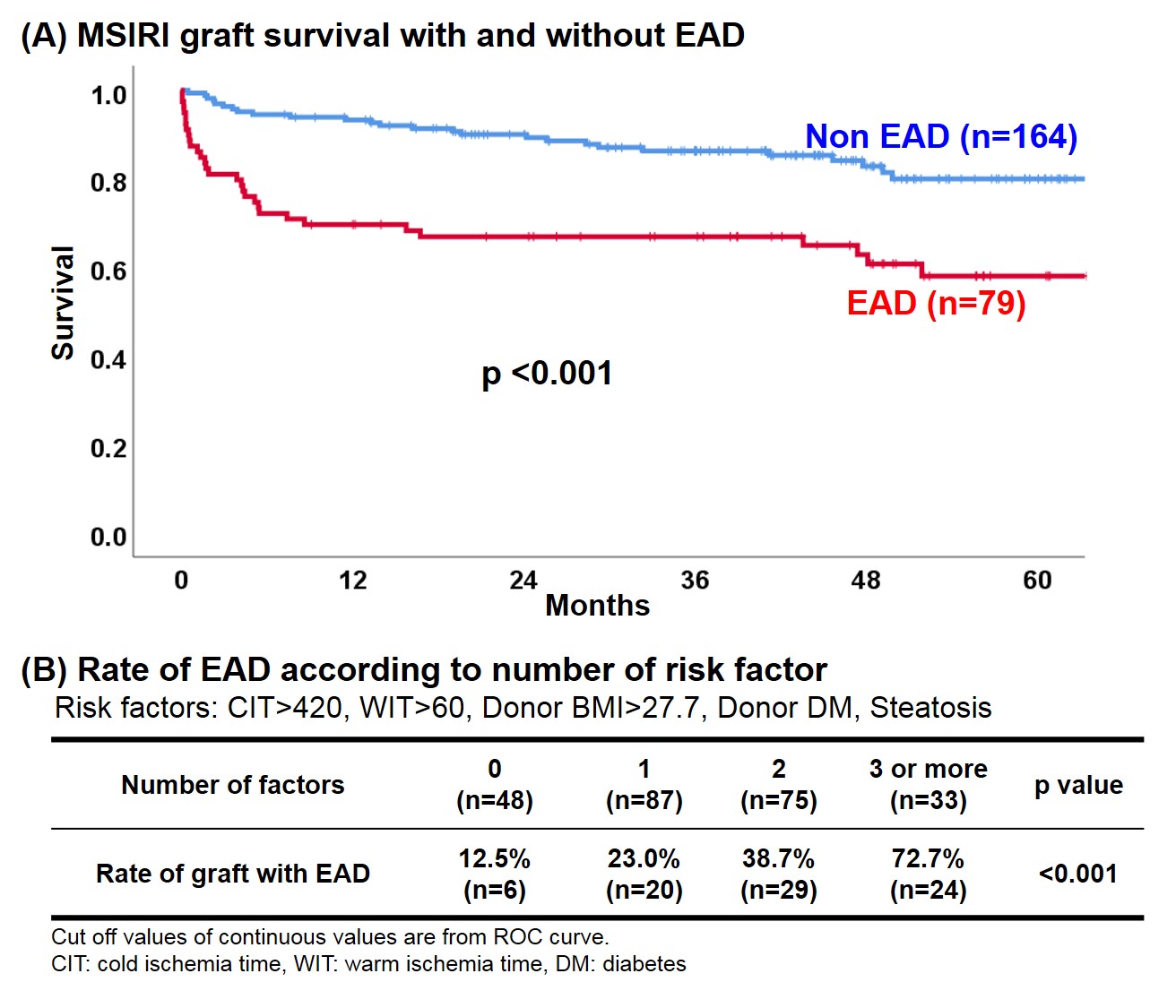
*Results: Among 492 grafts, 243 (49.4%) had MSIRI. These grafts had higher levels of maximal serum transaminases (AST: 1081 vs 752 IU/l, p<0.001, ALT: 539 vs 405 IU/l, p=0.002), and a higher rate of EAD (32.5 vs 20.5%, p=0.002). MSIRI grafts with EAD (n=79) had significantly poorer survival than grafts with MSIRI but no EAD (n=164) (Figure A). Longer cold ischemia time (OR: 1.003, p=0.006), longer warm ischemia time (OR: 1.028, p=0.027), steatosis with 20% or more large droplet cell (OR: 4.130, p=0.001), higher donor BMI (OR: 1.053, p=0.032), and donor diabetes (OR: 2.577, p=0.047) were identified as independent risk factors for EAD. The rate of EAD in MSIRI grafts with 3 or more risk factors was 72.7%, compared to12.5% in grafts with no risk factors (Figure B).
*Conclusions: EAD in the setting of MSIRI portends inferior graft outcomes compared to grafts with MSIRI alone. We identified cold ischemia time >420 min. and warm ischemia time >60 min, donor BMI>27.7, donor diabetes, and large droplet steatosis>20% as risk factors for the development of EAD in grafts developing MSIRI. Awareness of these factors in the setting of grafts with MSIRI associated EAD may guide patient management and if necessary timely graft replacement.
To cite this abstract in AMA style:
Ito T, Aziz J, Agopian VG, Younan S, DiNorcia J, Yersiz H, Farmer DG, Busuttil RW, Kaldas FM. Early Allograft Dysfunction in the Setting of Histologic Ischemia Reperfusion Injury Following Liver Transplantation: Analysis of Predictors and Outcomes [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/early-allograft-dysfunction-in-the-setting-of-histologic-ischemia-reperfusion-injury-following-liver-transplantation-analysis-of-predictors-and-outcomes/. Accessed February 22, 2026.« Back to 2019 American Transplant Congress