Donor Organ Resident M2 Type Myeloid Cells Protect Murine Orthotropic Liver Transplants from Ischemia and Reperfusion Injury
The Dumont-UCLA Transplant Ctr., UCLA, Los Angeles, CA.
Meeting: 2015 American Transplant Congress
Abstract number: 507
Keywords: Inflammation, Ischemia, Liver transplantation, Mononuclear leukocytes
Session Information
Session Name: Concurrent Session: Strategies To Minimize Ischemia Reperfusion Injury
Session Type: Concurrent Session
Date: Tuesday, May 5, 2015
Session Time: 4:00pm-5:30pm
 Presentation Time: 4:48pm-5:00pm
Presentation Time: 4:48pm-5:00pm
Location: Room 119-B
Liver ischemia reperfusion injury (lRI) is mediated by a pro-inflammatory immune response initiated by the activation of liver non-parenchymal innate immune cells, such as Kupffer cells (KCs). In liver transplantation (Tx) setting, as both donor resident KCs and recipient's infiltrating macrophages are present in the graft early post Tx, the question of whether donor or recipient's macrophages play roles in the pathogenesis of liver IRI remains controversial. As macrophages can be differentiated in to either pro-inflammatory M1 or anti-inflammatory/reparative M2 types, the potential therapeutic utility of M2 macrophages to protect transplants from IRI has not been explored. In this study, we took advantage of our recent finding that Phosphatase and Tensin Homolog (PTEN) gene deficient macrophages were the M2 type (Yue et al. J. Immunol, 192:5343), capable of protecting livers from partial warm IRI, and tested their function as either donor or recipient's myeloid cells (Lyz2-Cre+/- PTEN-loxP+/+) in a mouse model of liver cold storage (20h at 4°C) followed by orthotropic liver transplantation (OLT). The interaction of PTEN KO and WT macrophages in their TLR responses was studied in vitro. Although, the pro-inflammatory activation of WT cells was not significantly inhibited by co-cultured KO cells, culture supernatants from activated PTEN KO macrophages inhibited pro-inflammatory activation of WT cells; while culture supernatants from activated WT macrophages also partially reversed anti-inflammatory phenotype of PTEN KO cells. In vivo, liver IRI, as well as intragraft pro-inflammatory gene expressions, measured at both 6 and 24h post Tx was significantly decreased in only WT recipients of myeloid PTEN KO liver grafts (KO-WT), but not myeloid PTEN KO recipients of WT liver grafts (WT-KO) (Fig.). These data provide us evidence that donor resident KCs played a major role in IRI of OLTs, and their functional manipulation may represent a novel therapeutic strategy to ameliorate liver IRI in transplant patients. 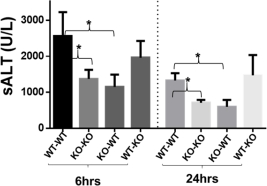
To cite this abstract in AMA style:
Yue S, Shen X, Gao F, Busuttil R, Kupiec-Weglinski J, Zhai Y. Donor Organ Resident M2 Type Myeloid Cells Protect Murine Orthotropic Liver Transplants from Ischemia and Reperfusion Injury [abstract]. Am J Transplant. 2015; 15 (suppl 3). https://atcmeetingabstracts.com/abstract/donor-organ-resident-m2-type-myeloid-cells-protect-murine-orthotropic-liver-transplants-from-ischemia-and-reperfusion-injury/. Accessed March 4, 2026.« Back to 2015 American Transplant Congress
