Consideration of the Futility of Transplant: 50% Mortality at 5 Years
Baylor University Medical Center, Dallas, TX.
Meeting: 2015 American Transplant Congress
Abstract number: C116
Keywords: Allocation, Graft failure, Liver transplantation, Survival
Session Information
Session Name: Poster Session C: Liver Donation and Allocation
Session Type: Poster Session
Date: Monday, May 4, 2015
Session Time: 5:30pm-6:30pm
 Presentation Time: 5:30pm-6:30pm
Presentation Time: 5:30pm-6:30pm
Location: Exhibit Hall E
Introduction: Transplant recipients are globally sicker at the time of liver transplantation (LT) in the current era. We sought to devise and validate a model to identify subjects with 50% mortality at 5 years after LT.
Methods: We examined data from the SRTR (2002-11) on adult primary LT recipients with MELD >25 and non-HCV diagnosis and excluded dual organ, retransplant, and MELD exception patients. We selected a priori recipient factors associated with worse patient survival. Model was developed on 70% of available SRTR data; internal validation was performed on 30% of the SRTR data and external validation was performed on center data (1985-2013). Risk factors selected in the final model were assigned points based on transformation of the regression coefficients with survival tree analysis to determine optimal cutoffs.
Results: On multivariable analysis, recipient factors and assigned points included: recipient age >60 (4 pts; HR 1.7, 95% CI 1.5-1.9), diabetes (2 pts; HR 1.3, 95% CI 1.1-1.6), creatinine >1.5mg/dL without hemodialysis (1 pt; HR 1.2, 95% CI 0.99-1.4), hemodialysis (3 pts; HR 1.7, 95% CI 1.4-2.1), and ventilator support (4 pts; HR 1.8, 95% CI 1.5-2.2). 5 year patient survival based on cumulative points (any combination) was 82.4% (0-4), 69.0% (5-7) and 50.9% (>7). Receipt of an “optimal” donor (age<50, non DCD, CIT<10h) attenuated 5 year patient survival for highest risk recipients (>7 points), 60.4% vs. 36.7% for sub-optimal donor. Similar findings were obtained on internal validation (SRTR, c statistic 0.81) and external validation (center data, c statistic 0.77). In center specific data, subjects with ≥ 7 points (vs. 0-4) had longer median initial hospitalization (15.5 vs. 8.5 days, p<0.001), longer ICU days (6.0 vs. 2.5 days, p<0.001) and more frequent re-admissions within the first year (55% vs. 49%, p=0.65).
Conclusion: Combination of relevant recipient factors may identify transplant candidates with sub-optimal outcomes, with implications on listing practices. Though urgency of transplant and reduction of geographic disparity are the cornerstones of the final rule, the “futility of transplant” needs to be reconsidered.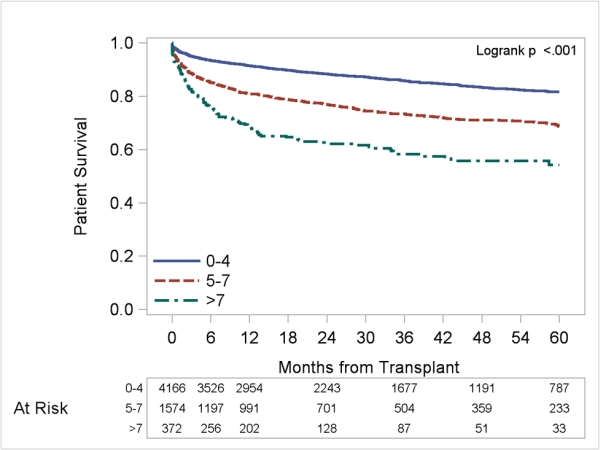
To cite this abstract in AMA style:
Asrani S, Saracino G, O'Leary J, Klintmalm G, Trotter J. Consideration of the Futility of Transplant: 50% Mortality at 5 Years [abstract]. Am J Transplant. 2015; 15 (suppl 3). https://atcmeetingabstracts.com/abstract/consideration-of-the-futility-of-transplant-50-mortality-at-5-years/. Accessed July 18, 2025.« Back to 2015 American Transplant Congress
