Clinical Outcomes of Living versus Deceased Donor Liver Transplantation for Primary Sclerosing Cholangitis: A Multicenter 15 Year Experience
O. Y. Mousa1, K. D. Watt1, J. K. Heimbach2, A. P. Keaveny3, J. E. Eaton1, D. M. Harnois3, B. Taner3, E. J. Carey4, A. A. Moss4, C. B. Rosen5, T. Taner5
1Department of Gastroenterology and Hepatology, Mayo Clinic, Rochester, MN, 2Department of Surgery, Mayo Clinic, Rochester, MN, 3Department of Transplant, Mayo Clinic, Jacksonville, FL, 4Department of Transplant, Mayo Clinic, Scottsdale, AZ, 5Department of Transplant, Mayo Clinic, Rochester, MN
Meeting: 2019 American Transplant Congress
Abstract number: B333
Keywords: Liver transplantation, Living-related liver donors, Primary sclerosing cholangitis, Survival
Session Information
Session Name: Poster Session B: Liver: Living Donors and Partial Grafts
Session Type: Poster Session
Date: Sunday, June 2, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall C & D
*Purpose: MELD-based allocation is known to reduce access to deceased donor liver transplantation (DDLT) for patients with primary sclerosing cholangitis (PSC). Living donor liver transplantation(LDLT) provides improved access and shorter waiting time for such patients. There is limited data on long term outcomes of PSC patients who underwent LDLT compared to DDLT.
*Methods: 441 patients from 3 academic centers underwent LT for PSC between 1/1/2002 and 12/31/2016. Children (<18 yr), cholangiocarcinoma or hepatocellular carcinoma, and those with prior LT were excluded (153 patients). Kaplan-Meier survival analysis and log-rank comparisons based on the type of organ donation were performed.
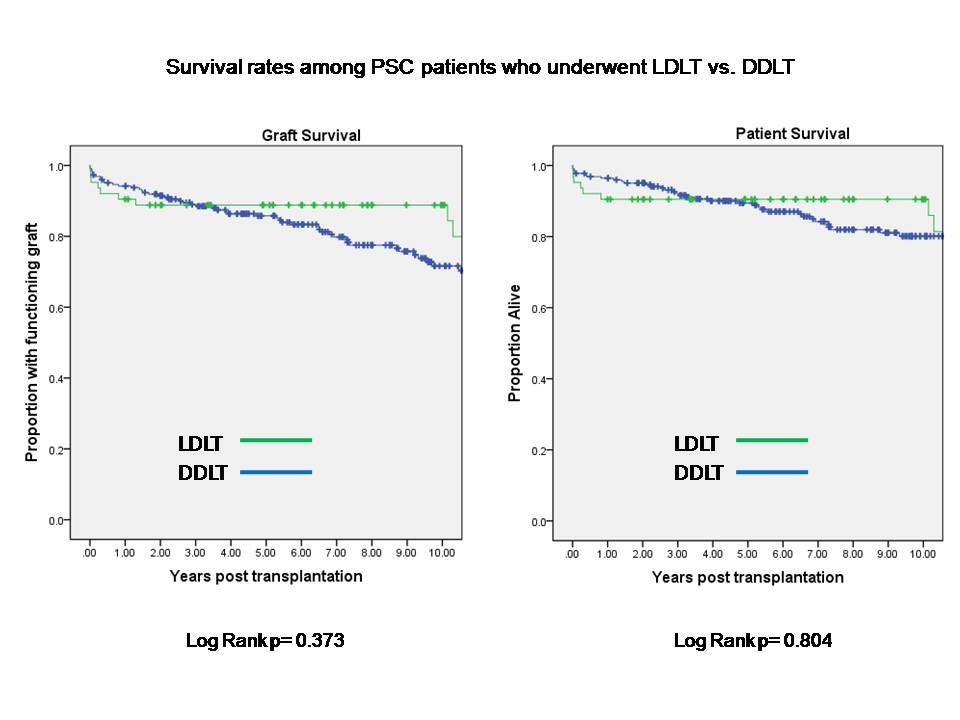
*Results: Of the 288 patients, 21.9% (63/288) underwent LDLT. Overall, LDLT patients were younger (41.6±14.4 vs. 50.9±13.3 yr; p=0.001 [95% CI 5.6-13.1]), and had lower MELD at transplant (15.9±5.2 vs. 21.7±7.0; p=0.001 [95% CI 3.9-7.7]). The donor age was lower in LDLT (39.0±11.0 vs. 48.3±21.3 yr; p=0.001 [95% CI 3.8-14.8]. Recipient sex and BMI were not different (60.3% vs. 65.8% male, and 24.9±4.7 vs. 26.2±5.6, respectively). Overall survival at 3, 5 and 10 years were 90.5%, 90.5% and 86% after LDLT, and 91.6%, 89.5% and 80% after DDLT. Graft survival at 3, 5 and 10 years were 88.8%, 88.8% and 79.9% after LDLT, and 88.5%, 85.8% and 71.6% after DDLT. Kaplan-Meier patient survival distributions were not statistically different among those who received LDLT compared to those who received DDLT (log-rank p=0.804). Similarly, graft survival distributions were not statistically different (log-rank p=0.373) (Figure).
*Conclusions: Patient and graft survival rates are high among PSC patients undergoing LDLT and are comparable to those of DDLT. This study demonstrates excellent long term outcomes after 10 years among LDLT recipients for PSC.
To cite this abstract in AMA style:
Mousa OY, Watt KD, Heimbach JK, Keaveny AP, Eaton JE, Harnois DM, Taner B, Carey EJ, Moss AA, Rosen CB, Taner T. Clinical Outcomes of Living versus Deceased Donor Liver Transplantation for Primary Sclerosing Cholangitis: A Multicenter 15 Year Experience [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/clinical-outcomes-of-living-versus-deceased-donor-liver-transplantation-for-primary-sclerosing-cholangitis-a-multicenter-15-year-experience/. Accessed July 18, 2025.« Back to 2019 American Transplant Congress