Clinical Factors That Determine the More Appropriate Induction Agent: ATG versus IL-2 Receptor Antagonists.
Johns Hopkins, Baltimore, MD.
Meeting: 2016 American Transplant Congress
Abstract number: C36
Keywords: Antilymphocyte antibodies, Induction therapy, Interleukin-2 receptor, Multivariate analysis
Session Information
Session Name: Poster Session C: Clinical Science - Kidney Immunosuppression: Induction Therapy
Session Type: Poster Session
Date: Monday, June 13, 2016
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Halls C&D
Antithymocyte globulin (ATG) is recommended over IL-2 receptor antagonist (IL2) in high-risk recipients for induction immunosuppression. However, “high-risk” status has not been defined in an evidence-based manner and the choice of induction agent depends on clinical judgment. We aimed to identify recipient subgroups that displayed distinctively superior or inferior survival with ATG versus IL2.
Methods: Using SRTR data, we studied 60,069 deceased-donor kidney transplant recipients between 2005-2014 who were prescribed ATG or IL2 for induction, in addition to a calcineurin inhibitor and antimetabolite for maintenance (considering steroid withdrawal as a potential confounder/effect modifier). We built Cox models for all-cause graft loss with interaction terms of ATG/IL2 and covariates.
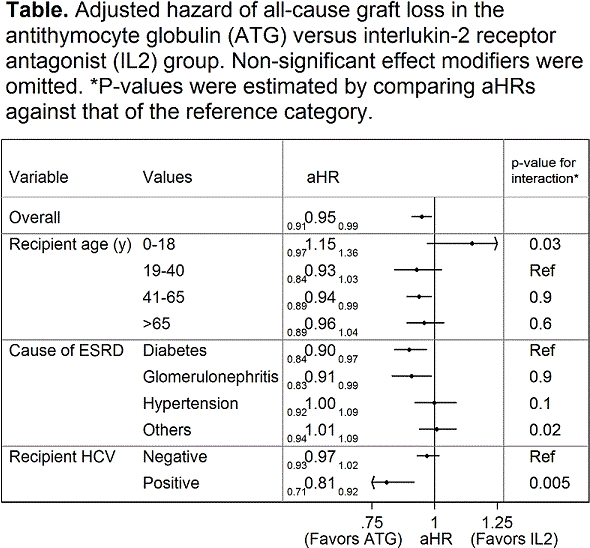
Results: Overall, ATG was associated with decreased hazard of graft loss compared with IL2 (aHR=0.910.950.99). However, the effectiveness of ATG on graft survival varied by recipient age, cause of ESRD, and HCV status. ATG was associated with a suggestively lower hazard of graft loss (aHR=0.840.931.03) among young adults (19-40y), but with a suggestively higher hazard (aHR=0.971.151.36)among pediatric recipients (0-18y; p-value for interaction=0.03). The impact of ATG versus IL2 also varied by cause of ESRD, with a greater value of ATG seen in those with ESRD due to diabetes or glomerulonephritis (aHR=0.840.900.97 and 0.830.910.99) than in those with ESRD due to hypertension or other causes (aHR=0.921.001.09 and 0.941.011.09; Table). ATG was associated with a significantly lower hazard of graft loss (aHR=0.710.810.92) among HCV(+) recipients, but not (aHR=0.930.971.02) among HCV(-) recipients (p for interaction=0.005).
Conclusion: Recipient age, cause of ESRD, and HCV status may need to be considered when choosing induction agent. These findings may help inform clinical judgment of induction choice in a more data-driven manner than is currently practiced.
CITATION INFORMATION: Bae S, Massie A, DiBrito S, Luo X, Kucirka L, Al Ammary F, Segev D. Clinical Factors That Determine the More Appropriate Induction Agent: ATG versus IL-2 Receptor Antagonists. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Bae S, Massie A, DiBrito S, Luo X, Kucirka L, Ammary FAl, Segev D. Clinical Factors That Determine the More Appropriate Induction Agent: ATG versus IL-2 Receptor Antagonists. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/clinical-factors-that-determine-the-more-appropriate-induction-agent-atg-versus-il-2-receptor-antagonists/. Accessed February 23, 2026.« Back to 2016 American Transplant Congress
