Cellular And Molecular Characteristics Of Intra-graft Lymphoid Aggregates In Chronic Lung Allograft Dysfunction
E. Miyamoto1, S. Juvet1, D. Hwang2, S. Keshavjee1, T. Martinu1
1Toronto Lung Transplant Program, University Health Network, Toronto, ON, Canada, 2Sunnybrook Health Sciences Centre, Toronto, ON, Canada
Meeting: 2019 American Transplant Congress
Abstract number: C324
Keywords: B cells, Graft-infiltrating lymphocytes, Lung transplantation, Lymphocyte activation
Session Information
Session Name: Poster Session C: Lung: All Topics
Session Type: Poster Session
Date: Monday, June 3, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall C & D
*Purpose: Lymphoid aggregates (LAs) have been identified within lung allografts post lung transplant (LTx). However, it remains controversial whether they represent benign lymphoid tissue or immunologically-active tertiary lymphoid organs (TLOs) and whether they participate in rejection processes, tolerance or both. We aimed to assess in detail the B and T cell component and clarify the specific molecular expression of LAs within lungs affected by chronic lung allograft dysfunction (CLAD).
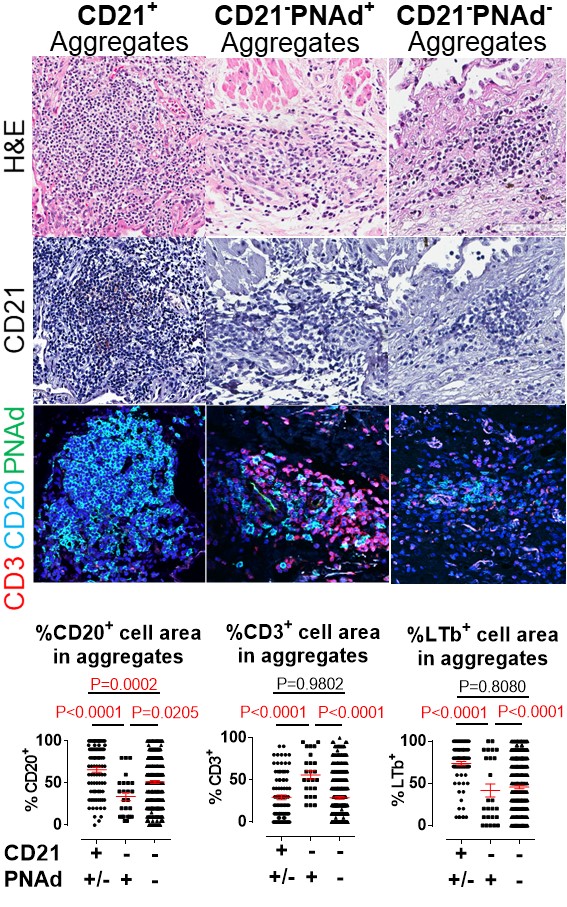
*Methods: We restrospectively reviewed 46 patients who underwent a 2nd LTx due to CLAD between March 2008 and Aug 2018 at our institution. We cut sequential 5 um sections of formalin-fixed paraffin-embedded explanted lung tissue for hematoxylin-eosin, immunohistochemistry (CD21, BCL6, Lymphotoxin-beta; LTb) and immunofluorescence (CD3, CD20, PNAd) staining (Figure).
*Results: The time interval between 1st LTx and CLAD was 38.1 ± 37.9 months and time from 1st to 2nd LTx was 64.1 ± 51.7 months. We assessed 600 intra-pulmonary LAs >= 1.0×104 um2 (13.3 ± 17.2 LAs per CLAD patient). Compared with 10 healthy donor lung samples, LAs were found much more frequently in CLAD lungs (28.2 ± 38.4 x 103 n/mm2 compared to 2.5 ± 4.2 x 103 n/mm2; p=0.0003). While the sizes of LAs were similar between CLAD and healthy lungs, LAs in CLAD lungs were less dense compared to healthy lungs (7.5 ± 3.0 x 103 cells/mm2 vs. 10.6 ± 3.9 x 103 cells/mm2, p=0.0395). A reticular CD21+ follicular dendritic cell staining pattern was positive in 21.4% of CLAD lung LAs compared to 60% in healthy lungs. Within CLAD lungs, compared to CD21– LAs, the CD21+ LAs had a higher percentage of CD20+ B cells, as well as cells staining positive for LTb and BCL6, molecules involved in follicular B and T cell development. CLAD lung CD21– LAs were assessed for PNAd+ high endothelial venules (HEV), characteristic of TLOs. The majority of CLAD lung LAs were CD21–PNAd– (72.8%) and a minority CD21–PNAd+ (5.9%). CD21–PNAd+ CLAD lung TLOs contained greater proportions of CD3+ T, less CD20+ and less LTb+ cells than CD21–PNAd–. Within CD21– LAs, positive BCL6 staining correlated with more T cells.
*Conclusions: CLAD lung LAs can be broadly categorized into CD21+, CD21–PNAd+, and CD21–PNAd– LAs. The CD21+ B cell-rich LAs have strong LTb and BCL6 staining, consistent with highly-organized active lymphoid structures. CD21–PNAd+ LAs have the highest proportion of T cells. Future studies should assess whether these distinct LAs play differential roles in post-LTx immune responses.
To cite this abstract in AMA style:
Miyamoto E, Juvet S, Hwang D, Keshavjee S, Martinu T. Cellular And Molecular Characteristics Of Intra-graft Lymphoid Aggregates In Chronic Lung Allograft Dysfunction [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/cellular-and-molecular-characteristics-of-intra-graft-lymphoid-aggregates-in-chronic-lung-allograft-dysfunction/. Accessed February 21, 2026.« Back to 2019 American Transplant Congress