Causal Relationship between Anti-Thymocyte Globulin Induction Therapy and Development of Monomorphic PTLD in Renal Transplant Recipients
1Medicine, Medical University of South Carolina, Charleston, SC, 2Medicine, Royal Stoke, Royal Stoke, United Kingdom, 3Medicine, Cairo University, Cairo, Egypt, 4Medicine, University of Liverpool, Liverpool, United Kingdom
Meeting: 2020 American Transplant Congress
Abstract number: C-213
Keywords: Antilymphocyte antibodies, Induction therapy, Infection, Post-transplant lymphoproliferative disorder (PTLD)
Session Information
Session Name: Poster Session C: PTLD/Malignancies: All Topics
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: The aim of our study is to explore the causality between ATG and different types of post-transplant lymphoproliferative disorder (PTLD) in renal transplant recipients (RTR).
*Methods: All patients diagnosed with PTLD post-renal transplant in U.S. Organ Procurement and Transplantation Network from 2000-2015 were retrospectively reviewed. Data including type of PTLD, recipient and donor age, type of induction therapy, maintenance immunosuppression medications, sex, ethnicity, donor type, PRA, cold ischemia time, HLA mismatches, EBV status, CMV, HBV, HCV and HIV status were collected. Multivariate logistic regression analysis was used to assess risk factors for different types of PTLD. Inverse probability weights were used to adjust confounders among different groups using propensity score analysis. Treatment effects model was used to assess relation between ATG induction therapy and different types of PTLD. Bradford Hill’s criteria for causality of a certain variable to specific outcome has been used to identify the causality of ATG to monomorphic PTLD.
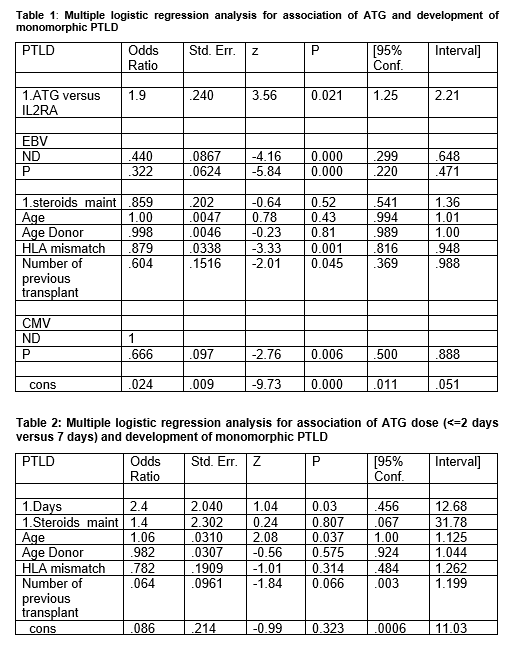
*Results: Of the 2345 PTLD RTR identified, more than half (59.6%) had monomorphic PTLD type. Multivariate regression analysis showed that compared to IL-2 receptor antagonist, ATG induction therapy was significantly associated with increased risk of monomorphic PTLD (P=0.021, OR=1.9, 95% CI: 1.25, Table 1). Treatment effects model using inverse probability weights showed that ATG was significantly associated with increased risk of monomorphic PTLD after adjustment of all other confounders (P=0.042). In addition, patients who received ATG daily for 7 days after transplant had higher risk of developing monomorphic PTLD in comparison to those who received ATG daily for ≤2 days post-transplant (P=0.03, OR: 2.4; 95% CI: 0.45, Table 2).
*Conclusions: The association and dose-response relationship between ATG induction therapy and subsequent development of monomorphic PTLD in RTR is strongly suggestive of causality.
To cite this abstract in AMA style:
Soliman K, Ali H, Fulop T, Osman A, Halawa A. Causal Relationship between Anti-Thymocyte Globulin Induction Therapy and Development of Monomorphic PTLD in Renal Transplant Recipients [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/causal-relationship-between-anti-thymocyte-globulin-induction-therapy-and-development-of-monomorphic-ptld-in-renal-transplant-recipients/. Accessed February 17, 2026.« Back to 2020 American Transplant Congress