Calculated Panel Reactive Antibody Values Increase for Kidney Transplant Candidates with HLA-DQA and HLA-DPB Unacceptable Antigens
1Cedars-Sinai Heart Institute, Beverly Hills, CA, 2Immunogenetics Lab, Southwest Immunodiagnostics, Inc., San Antonio, TX, 3Bioinformatics Research, Be The Match/National Marrow Donor Program, Minneapolis, MN, 4Department of Pathology, Tulane University School of Medicine, New Orleans, LA
Meeting: 2020 American Transplant Congress
Abstract number: 109
Keywords: Alloantibodies, Histocompatibility, Histocompatibility antigens, Major histocompatibility complex (MHC)
Session Information
Session Name: Histocompatibility and Immunogenetics
Session Type: Oral Abstract Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:45pm
 Presentation Time: 4:27pm-4:39pm
Presentation Time: 4:27pm-4:39pm
Location: Virtual
*Purpose: Calculated panel-reactive antibody (CPRA) is the official metric of sensitization used by the United Network for Organ Sharing (UNOS) for kidney allocation. CPRA includes unacceptable antigens (UA) at the HLA-A, -C, -B, -DRB1, and -DQB1 loci but does not include the HLA-DQA1 or -DPB1 loci. We sought to determine the effect of including HLA-DQA1 and -DPB1 locus UA on CPRA values for sensitized kidney transplant candidates.
*Methods: A cohort of kidney transplant candidates added to the wait list from the introduction of the new kidney allocation system 2014-12-04 through 2018-12-31 with >= 1 UA was obtained from UNOS (n=63,151). A CPRA calculator including all 11 HLA loci was developed using HLA typing collected by the National Marrow Donor Program. For each candidate, the CPRA value computed using the NMDP 11 locus calculator (11L-CPRA) was compared to the value computed using the current UNOS 5 locus calculator (5L-CPRA). The maximum 5L-CPRA value during listing was used for each candidate. The prototype 11-locus NMDP CPRA calculator is available at http://transplanttoolbox.org.
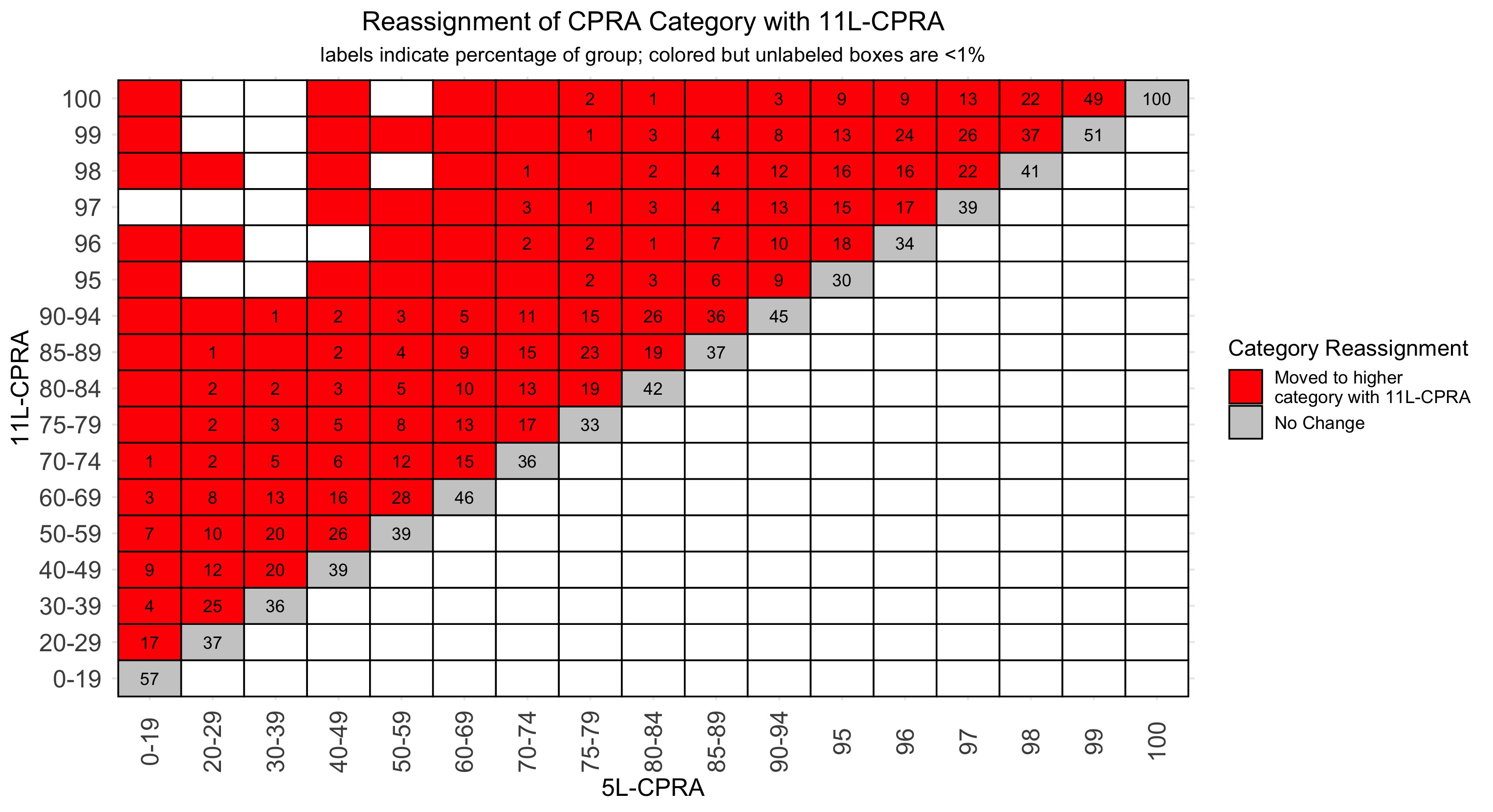
*Results: In candidates with any UA, 12.0% had HLA-DQA1, 13.4% had HLA-DPB1, and 3.3% had both loci. In candidates with HLA-DQA1 and/or -DPB1 UA, the median 5L-CPRA was 71.1%, which increased to 82.7% with the additional loci. The median increase in CPRA was 1.8% (IQR 0.0 – 12.5) and 7,526 (56%) candidates had an increase >= 1%. Based on the 11L-CPRA value, 5,968 (45%) candidates moved to a higher CPRA category and 7,440 (55%) did not change categories (FIGURE).
*Conclusions: The addition of the HLA-DQA1 or -DPB1 loci leads to an increase in CPRA for many candidates with these UA, which in turn leads to a significant reclassification of allocation priority by CPRA category. We anticipate that implementation of a more comprehensive CPRA metric that includes HLA-DQA1 and -DPB1 would improve equity in allocation for candidates with UA at these loci.
To cite this abstract in AMA style:
Kransdorf EP, Murphey C, Maiers M, Gragert L. Calculated Panel Reactive Antibody Values Increase for Kidney Transplant Candidates with HLA-DQA and HLA-DPB Unacceptable Antigens [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/calculated-panel-reactive-antibody-values-increase-for-kidney-transplant-candidates-with-hla-dqa-and-hla-dpb-unacceptable-antigens/. Accessed February 16, 2026.« Back to 2020 American Transplant Congress