Association between Pre-Transplant Frailty and Increased Length of Stay after Lung Transplantation
David Geffen School of Medicine at UCLA, Los Angeles, CA
Meeting: 2020 American Transplant Congress
Abstract number: B-292
Keywords: Age factors, Elderly patients, Length of stay, Lung transplantation
Session Information
Session Name: Poster Session B: Lung: All Topics
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Given the growing numbers of older lung transplant candidates, there has been increasing interest in using frailty assessment for risk stratification of transplant candidates. We evaluated physical frailty in lung transplant candidates to determine whether frailty is associated with adverse patient outcomes.
*Methods: Lung transplant candidates ages 60 and up were evaluated in the outpatient setting by Fried Frailty Phenotype (FFP) and the Short Physical Performance Battery (SPPB) under an IRB-approved study. The FFP score assesses weight loss, fatigue, and physical activity, and measures gait speed and grip strength. The SPPB score is based on gait speed, balance, and lower extremity strength. Cognitive testing and screen for depression were also performed.
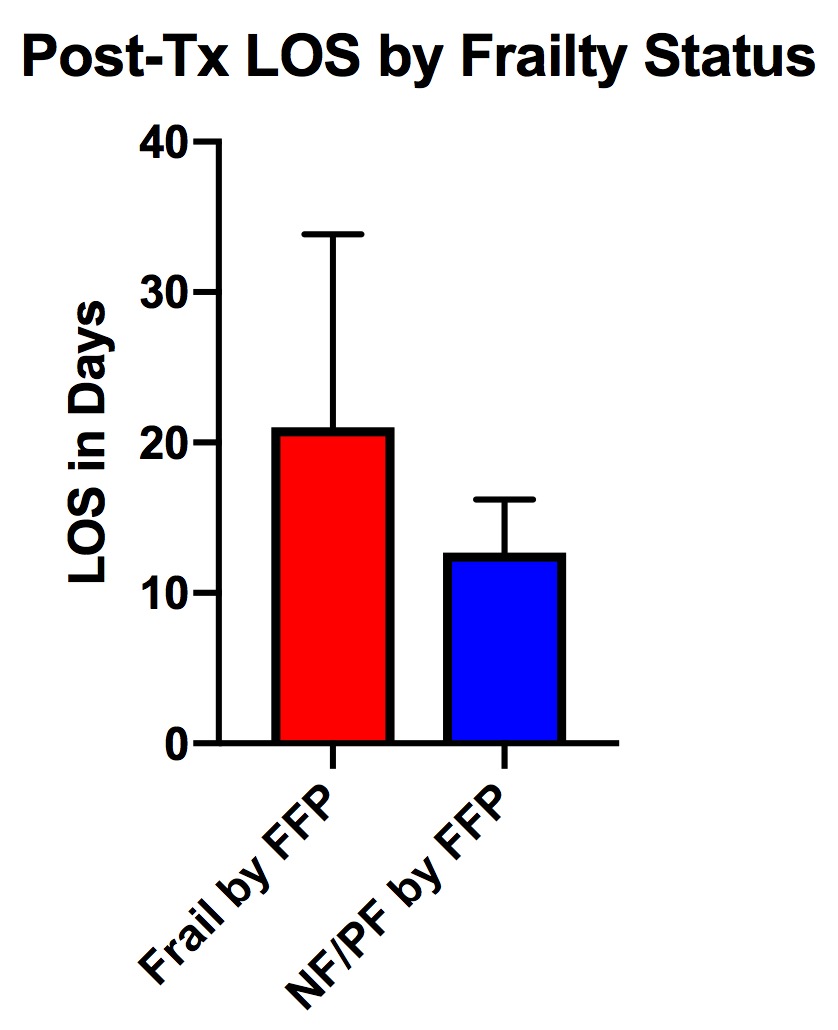
*Results: Both FFP and SPPB were measured in 45 subjects. Of these patients, 26 were frail (58%), 18 were pre-frail (40%), and 1 was non-frail (2%) by FFP, while 2 were frail (4%), 29 were pre-frail (64%), and 14 were non-frail by SPPB (31%). Patients classified as frail by FFP demonstrated a higher LAS score than pre-frail or non-frail patients (p=0.004), who were also more likely to have a lower (worse) SBBP score (p=0.014), but there was no significant difference by chronologic age (Table). There was a trend towards increased rates of transplantation in frail patients. Interestingly, the median length of stay (LOS) was significantly longer for frail patients (16.5 v 12 days, p=0.35) (Figure). A similar trend was seen for frailty by SPPB score, although this did not reach statistical significance (16 v. 12 days, p=0.181). Although LAS score was also predictive of longer LOS (p=0.009), chronological age was not (p=0.462).
*Conclusions: Measurement of frailty in lung transplant candidates may offer the ability to improve prediction of adverse clinical outcomes including increased length of stay after transplantation. This information is distinct from the information provided by chronological age. Collection of frailty information at the time of candidate evaluation can help to direct resources to improve clinical outcomes. Future studies will evaluate how frailty changes after transplantation.
| Age (range) | Frail (n=26) | Non-Frail/PF (n=19) | p-value |
| Age (range) | 65 (61-72) | 66 (60-71) | 0.774 |
| Female sex | 42% | 37% | 0.712 |
| LAS | 44 (28-75) | 35 (33-43) | 0.004 |
| SPPB (range) | 8 (6-11) | 9 (6-12) | 0.014 |
| Transplanted | 69% | 47% | 0.097 |
| LOS (range) | 16.5 (9-46) | 12 (8-19) | 0.035 |
| Death | 23% | 11% | 0.277 |
To cite this abstract in AMA style:
Schaenman J, Ventigan N, Huang J, Jaladanki S, Shih L, Gee S, Sayah D, Weigt SS, Ardehali A, Biniwale R, Goldwater D. Association between Pre-Transplant Frailty and Increased Length of Stay after Lung Transplantation [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/association-between-pre-transplant-frailty-and-increased-length-of-stay-after-lung-transplantation/. Accessed July 14, 2025.« Back to 2020 American Transplant Congress